Osteoporosis is a condition that causes bones to get weaker over time and break more easily, which can lead to complications. About 10 million people ages 50 and older have osteoporosis in the United States. This is especially true after menopause when the body produces less of the hormone estrogen, which helps to maintain bone density. During this time, it is important to screen for osteoporosis to help diagnose it early.
Bones grow and add more density until we’re about 25. Then they stay about the same with equal amounts of breakdown and new growth. But after age 50, we experience more bone breakdown than new growth.
While typically there are no noticeable symptoms of osteoporosis, the first sign might be a fracture after bones become weak. Osteoporosis is a common cause of fractures in older people, so regular screenings to check bone density are essential to treat osteoporosis and prevent fractures.
In people who have gone through menopause and have no other risk factors or a history of fractures, Sarah Musleh, MD, a Dallas-based endocrinologist and co-founder of Anzara Health, says that screening guidelines recommend that osteoporosis screening through bone measurement tests begin at age 65. Musleh also notes that low testosterone levels or chronic kidney disease—conditions that can lead to low bone density in males—may also be reasons for bone measurement tests.
The first step in getting a diagnosis is a physical exam, where your healthcare provider will ask questions about your health history. Questions might include:
- Have you had any stress fractures before?
- Has anyone in your family ever been diagnosed with osteoporosis or fallen and fractured a hip?
- Do you smoke cigarettes?
- How often do you drink alcohol?
- What’s your typical diet like?
- Does it include enough sources of calcium and vitamin D?
- How often do you exercise or get physical activity?
- What medications are you taking?
These questions help them understand your risk factors for developing the condition. For example, Dr. Musleh says smoking cigarettes or consuming large amounts of alcohol puts people at a higher risk of low bone density.
According to Kevin R. Stone, MD, an orthopedic surgeon at The Stone Clinic in San Francisco, one of the typical things healthcare provider look for in bone disorders is whether bone pain is present. If there is pain, Dr. Stone says the physical exam may include seeing if there’s pain with impact and whether it’s consistent with a stress fracture. These clues can be gathered through a test at your provider’s office.
“If they can hop on one leg and it [does] not produce sudden pain, that pretty much rules out most stress fractures,” says Dr. Stone. “If they have a subtle stress fracture in a hip or a shin or a foot, [once] they do a single-leg hop, it usually reproduces the pain.”
Once your healthcare provider has enough information from the exam, they’ll most likely order screening tests and labs to see bone density, nutrient and hormone levels, and anything else they feel will help give a complete picture of your bone health.
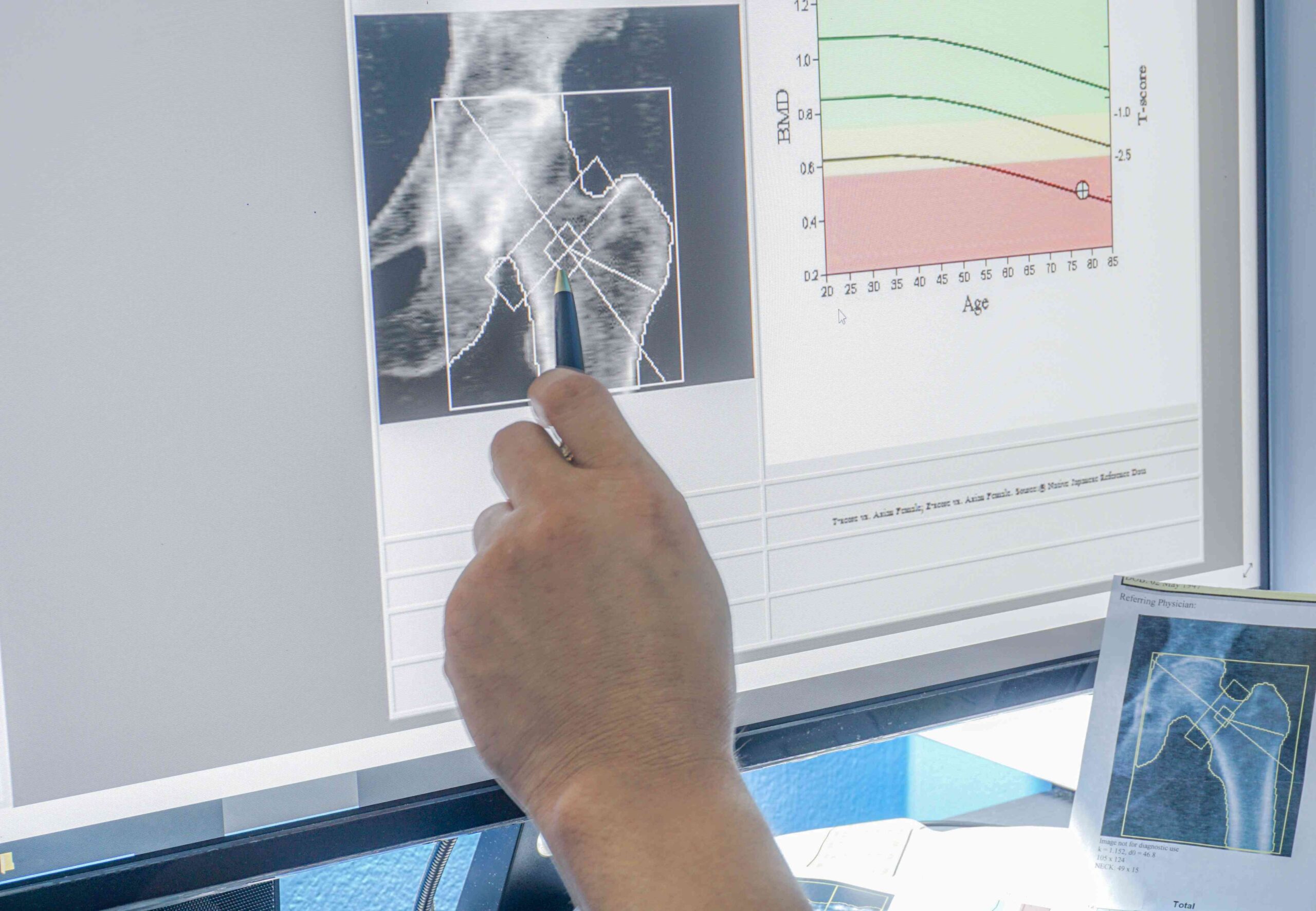
A bone mineral density test can measure how dense or strong your bones are and can be used to diagnose osteoporosis. The most frequently used diagnostic test is dual-energy X-ray absorptiometry (DEXA or DXA).
A DEXA scan is a test that uses low-dose X-rays to show the bone density at the hip, spine or wrist. This test is the gold standard for diagnosing osteoporosis, and if the scan is abnormal, this is an indicator of bone deficiency, says Dr. Stone.
Results from the DEXA are given through a scoring system called the T-score in which the results are compared to the bone mineral density of a healthy young adult. T-score levels include:
- Normal: T-score between +1 and -1
- Low bone mass: T-score between -1 to -2.5
- Osteoporosis: T-score of -2.5 or lower
- Severe osteoporosis: T-score of -2.5 or lower with one or more fractures
Other tests can check bone health, but they aren’t used as often as the DEXA. These tests include:
- Quantitative computed tomography (QCT): Gives a three-dimensional measurement of bone density at the hip and spine using higher radiation levels than a DEXA and measures bone mineral density of only the spongy bone inside the vertebra.
- Biomechanical computed tomography (BCT): Takes information from a CT scan of the hip or lower spine and uses it to measure bone density.
- Radiofrequency echographic multi-spectrometry (REMS): An ultrasound that measures bone density of the hip and spine.
- Tests at peripheral (non-spine, non-hip) sites: Tests used to measure bone density in areas other than the hip and spine, including arms, legs, fingers, wrists, and heels. Examples of these include pDEXA (peripheral dual-energy X-ray absorptiometry), pQCT (peripheral quantitative computed tomography), and QUS (quantitative ultrasound).
Extensive lab testing is used to build a picture of someone’s bone health, according to Dr. Musleh. This means going beyond checking vitamin D and calcium levels. Dr. Musleh says a blood test will also look at kidney function, parathyroid hormone levels, thyroid hormone levels, liver function, and blood counts. These measurements can be used to understand how much calcium is in the blood and how gland and organ function might contribute to osteoporosis.
Elevated calcium in the blood suggests hyperparathyroidism, and decreased calcium suggests malabsorption (difficulty absorbing nutrients from food) or a vitamin D deficiency, says Dr. Stone.
Hyperparathyroidism happens when the parathyroid glands make high amounts of the parathyroid hormone, which regulates calcium balance in the bloodstream and tissues. If that balance is not maintained and there’s too much calcium in the bloodstream and not enough in the bones, it can lead to osteoporosis.
Another test used to evaluate bone health, according to Dr. Stone is the 24-hour urinary calcium excretion test which measures how much calcium is in your urine.
When a person is older, they tend to be at a higher risk for fractures. Research shows that older adults over 65 are three to four times more likely to die within a year after having surgery for a hip fracture than younger people.
Dr. Musleh says it could be hard to recover after a hip fracture for people 70 and older. She explains that older people who have surgery for a broken hip could also be at risk for a urinary tract infection (UTI) and blood clots that could cause a pulmonary embolism or stroke during their hospital stay. So, it’s important to diagnose and treat osteoporosis in a person’s early 50s and 60s to strengthen bones or maintain bone density and try to prevent fractures.
Depending on your test results, treatment could involve preventing further bone density loss or rebuilding bone to compensate for severe bone loss.
Although calcium and vitamin D supplements may help, medications are frequently vital to treatment. “If you have osteoporosis and need treatment, calcium and vitamin D are additives to the pharmacotherapy,” say Dr. Musleh.
Dr. Stone also recommends resistance exercises as a vital part of treatment because bone responds to stress, resistance exercises such as walking up and down stairs, hiking, and lifting weights can slow bone loss, which starts after age 30.
The goal is to reduce the risk of having a fracture. “If your bones are as strong as we can get them, then hopefully you fall and you get a bruise, but you don’t get a fracture,” says Dr. Musleh.
When searching for a provider to diagnose and treat osteoporosis, she recommends looking for either a primary care doctor who specializes in bone health or an endocrinologist treating people with low bone density. Since osteoporosis is a chronic condition, Dr. Musleh says that having the right doctor can improve your chances of getting the proper treatment and understanding the process.
“If you took treatment, and now you’re off treatment, insist on getting a bone density check again in two or three years to make sure that the bones are still holding and the density is still good,” she says.
Osteoporosis, a condition causing bone weakness and increased fracture risk, affects millions of people, particularly post-menopausal women and those over 50. Screening using bone measurement tests usually starts around age 65. Diagnosis, which can be found through physical exams and DEXA scans, among other methods, helps to inform your treatment plan. This may include medications, exercises, and supplements to prevent fractures.
With aging, fracture risk rises significantly, particularly following hip fractures, leading to higher mortality rates in older adults. Early diagnosis and treatment can prevent fractures and related complications; this may involve regular monitoring of bone density every two to three years. Optimal care involves finding a healthcare provider who specializes in osteoporosis management to track progression and your treatment is right for you.