Abstract
The aim of this study was to assess the effect of nutrition education and counseling using health belief health model constructs along with iron-folic acid supplementation on hemoglobin level and adherence to IFAs during pregnancy. The study was a three-month quasi-experimental study design in Butajira town, Ethiopia. Community-based nutrition education and counseling sessions using the Health belief model, and IFAS for six weeks were given to the pregnant women. Compliance with iron-folic acid supplementation (IFAS) was assessed using pill counts based on the number of remaining pills in the retained prescribed bottles or strips. End-line data were collected from 97 interventions and 96 control groups of pregnant women after 6 weeks of nutrition education interventions. The analysis of the effect of the intervention was done using difference-in-difference and a generalized estimation equation (GEE) approach. At the end of the nutrition education intervention, there was a significant drop in the proportion of anemia in the intervention group compared to the control group. The prevalence of anemia among the intervention group declined from 27.8% at baseline to 7.2% after intervention. The change in the knowledge score regarding IFAS and maternal adherence to IFAS were significantly higher in the intervention group as compared to the control group (p < 0.001). In this study, the odds of adherence to IFA supplementation were 2.26 (95% CI 1.55 to 3.29) times higher among those who received nutrition education interventions as compared to the control group. Implementation of community-based nutrition education and counseling along with IFAS improved the hemoglobin level and adherence to IFAS among pregnant women. Therefore, there is need to integrate community-based nutrition education approach by using HBM constructs with antenatal IFAS distribution to improve supplementation and hemoglobin level of pregnant women.
Introduction
Anemia is one of the world’s most common public health problems. Globally, 38% of pregnant women and 29% of women of reproductive age are anemic, and relatively little progress has been made in reducing prevalence since 19951. Women and children in low- and middle-income countries (LMICs) are the most affected. Anemia is associated with poor birth outcomes, impaired cognitive development, and low productivity in adults2. Anemia in pregnant women increases the risk of having low birth-weight infants, preterm delivery, and maternal mortality3,4. Despite significant achievements in maternal and child health-related programs over the past decade, the prevalence of anemia among pregnant women has shown no reductions but slight increments over the past decade, from 22% in 2011 to 29.1% in 20165.
Currently, WHO recommends that pregnant women consume 60 mg of iron and 0.4 mg of folic acid per day for > 90 days to prevent the risk of maternal anemia, low birth weight, neural tube defect, and preterm birth6. Iron-folic acid supplementation (IFAS) increases hemoglobin levels thereby reducing prevalence of anemia and increasing the mean blood hemoglobin level by 10.2 g/l in pregnant women7,8. In addition, IFAS reduces the incidence of anemia by 69% and iron deficiency anemia by 66% at term9 as well as decreasing neonatal mortality by 34-45%10,11. Ethiopia has implemented programs that provide free, often with folic acid, ANC services. However, adherence to IFAS has remained low over the years and the prevalence of anemia in pregnant women remains persistently high in Ethiopia. For example, according to the 2016 Ethiopian demographic health survey, only 5% of pregnant mothers took an iron with a folic acid tablet for 90 days, and 58% of pregnant mothers did not take5. Several factors influence maternal adherence to IFAS, including socio-cultural circumstances, poor knowledge, a negative attitude, and poor awareness towards iron/folic acid deficiency12,13,14. Galloway et al. found, in an eight-country qualitative study, that inconsistent supply, inappropriate targeting, and inadequate counseling were the major barriers to adherence to IFAS15.
Nutrition education and counseling are widely used strategies to improve maternal nutritional status during pregnancy16. Evidence showed that health education intervention is an important tool to improve knowledge on anemia and adherence to the IFAS during pregnancy17,18. Community-based health education on anemia and IFAS has also proved successful in Cambodia, the Philippines, Vietnam and Kenya where improvements in awareness and knowledge of anemia and IFAS were reported19,20. A review study also suggested that nutrition education and counseling can improve both anemia outcomes and adherence to IFAS recommendations in low- and middle-income countries (LMIC)21. However, in Ethiopia, the routine nutrition education provided for pregnant women by the health extension workers is inconsistent, and counseling about possible side effects of IFAS and how to mitigate them is also missed most of the time22. Therefore, nutrition education and appropriate counseling during pregnancy seem to be of high priority to promote positive maternal and pregnancy outcomes21. In Ethiopia, data on the effect of community-based nutrition education and counseling using health belief model constructs along with IFAS on anemia and adherence to IFAS among pregnant women was scarce. Thus, the aim of this study was to assess the effect of community-based nutrition education and IFAS intervention on anemia and adherence to IFAS in pregnant women in southern Ethiopia.
Materials and methods
Study design
The details of the study methods adopted for this study was published elsewhere in other article23.
A quasi-experimental study was conducted among pregnant women who were in the second trimester (gestational ages less than 16 weeks), not suffering from any chronic illness, had no severe anemia and provided verbal consent to participate in the study. Pregnant women were recruited and assigned to receive nutrition education and IFAS in the intervention group and routine antenatal care services only in the control group by two stages. The study was performed as per the principles of Helsinki Declaration.
Study setting and sampling
The study was conducted in Butajira city administration located in 135 km southern part of Ethiopia. In 2022, the population of Butajira city administration is 89, 824 and has increased by 6.8% from 2007.
The sample size was determined by using the formula for comparison of two population proportions for the intervention and control groups.
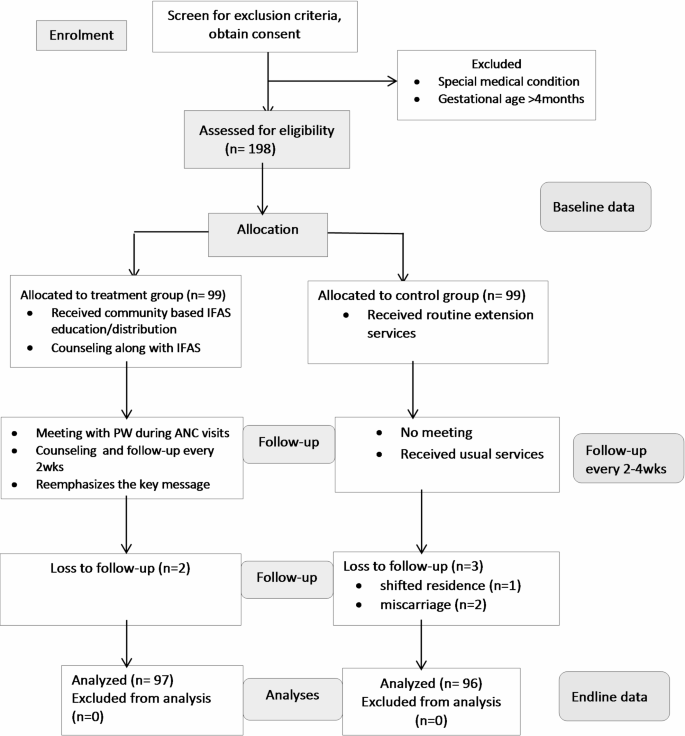
The following assumptions were considered when estimating the required minimum sample sizes: the expected proportion of pregnant women with good knowledge (P1) 0.77 and P2 was 0.5224. We wanted to detect an absolute increase of 25% in the intervention group at 5% significance level, and 80% power. The calculated sample size was multiplied by 1.5 to adjust for design effect and added 10% loss to follow up, the final sample size was 198. After assessing for eligibility, primary author randomly assigned pregnant women to the intervention and control groups in a 1:1 ratio using coin tossing (Fig. 1).
Data collection
The trained data enumerator collected data from pregnant women who gave written informed consent to participate in the study. The baseline data was collected using interviewer administered questionnaire. The questionnaires included socio-economic characteristics of women and their households, obstetric history, prenatal health seeking behavior, and measure variables relevant to maternal nutrition during pregnancy, IFA compliance level and biochemical assessment such as hemoglobin level estimation were done.
At the end of intervention, data on IFA compliance and hemoglobin status were collected. Compliance with the IFAS was assessed by pill count based on the number of remaining pills in the retained prescribed bottles. The number of unused pills in the retained pill bottles or strips was counted and recorded at the last visit following the last week of the intervention. If pregnant women were able to take at least ≥ 72 IFAS pills or 80% from the total take period, they were considered an adherent to the IFAS utilization, whereas those who were not able to take < 72 IFAS pills or < 80% from the total intake period were considered non-adherents to the IFAS intakes6.

Flow diagram showing the effect of community-based nutrition education and counseling targeting knowledge and attitude towards IFAS among pregnant women.
Hemoglobin was measured using a portable and battery-operated machine (HemoCue, Angel Holm, Sweden). After swiping the site with disinfectant, a finger prick was made to obtain blood for hemoglobin measurement. The first two drops were swapped away and the third drop was used to fill the micro cuvette for reading of the hemoglobin. Maternal anemia is defined as Hemoglobin value < 11 g/dl during pregnancy25.
The intervention
Nutrition education was delivered in Amharic. An organized work schedule, counseling cards, and nutrition education were provided to the intervention group. The core messages for the lessons were generated using the health belief model (HBM)26. It was modified in the recommendation to the Ministry of Health (MOH), Ethiopia27. The messages were framed in a way that addresses all components of HBM constructs like perceived susceptibility (the belief about the likelihood of developing a health problem or experiencing negative outcomes), perceived severity (the assessment of the seriousness or consequences of a health problem), perceived benefits (the belief about the positive effects of taking action to prevent or treat a health problem), perceived barriers (the belief about the costs or obstacles of taking action), cues to action (the factors that trigger or motivate action, such as symptoms, media messages, or social influences), self-efficacy (the confidence in one’s ability to perform a health behavior successfully). The health belief model was selected because the desired behavioral change is at an individual level and due to its convenience and simplicity.
For the intervention and control groups, baseline and endline assessments were collected. Following the gathering of baseline data, intervention groups were placed in groups at nearby village and received nutrition education regularly, once every two weeks, for a period of three months (six sessions) for 30 to 45 min per session. Four nurses with Bachelor of Science (BSc) degrees delivered nutrition education, while two Master of nutrition (MSc) specialists supervised the nutrition education sessions. The core contents of the session were: increasing knowledge about iron-rich food sources, iron-folic acid supplements (IFAS) (how to take the IFAS, when to take it, and how to absorb it more, foods rich in iron and folic acid, common side effects and their management; and enhancers/inhibitors of iron/folic absorption), iodized salt, meal frequency, and portion size with increasing gestational age; food groups; taking day rest; reducing heavy workloads; enhancers and inhibitors of iron absorption; increasing utilization of health services; and interrupting the intergenerational life cycle of malnutrition; increasing pregnant women’s perceptions of undernutrition and factors leading to it; poor eating practices causing inadequate dietary intake and disease; a diet adjustment.
Nutrition education sessions included presentations, discussions, demonstrations, and picture-based exercises. Key messages, realistic activities, and the GALIDRAA (greet, ask, listen, identify, discuss, recommend, agree, and make follow-up appointments) processes were all identified by the trainers as crucial counseling abilities. After the pregnant women were enrolled, reasonable attempts were made to encourage their retention and full follow-up for the duration of the trial by providing them with incentives to reduce missing data. Periodic conversations about compliance with the intervention during routine meetings and home visits by trainers served to retain interest in the study. Moreover, home visits were planned to lessen the strain of follow-up visits among pregnant women.
Intervention fidelity
The investigators developed criteria to assess the fidelity of the intervention based on the National Institutes of Health (NIH) Behavioral Change Consortium’s best practice recommendations28. The criteria used include research design, training of nutrition educators, intervention delivery, and receipt of intervention. To balance the variations, equal numbers of eligible participants were selected for the intervention and control groups. In addition, to reduce information contamination between the intervention and control groups, non-adjacent kebeles were selected. Intervention “dose” was adequately described and the same for each group in the study, which also included a comparison group and a counseling manual. To minimize between-educators variation, educators received instruction utilizing a manual, simulated counseling sessions, and ongoing supervision. Educators’ knowledge and skills were assessed by pre- and post-training tests and practical evaluation. Implementation of the intervention was assessed using post-intervention knowledge and attitude towards IFAS. Besides, each woman received an equal number and frequency of counseling, as well as the length of contacts within an intervention group to make the process standardized.
Outcome measure
The primary outcome for this study was the effect of nutrition education and IFAS on anemia level of pregnant women after three months of intervention. Secondary outcomes included the adherence to IFAS.
Data management and analysis
The data were entered, cleaned, coded, and analyzed using Statistical Package for Social Science version 26.0 software. The characteristics of respondents were also described in both the intervention and control groups. The wealth index was computed using principal component analysis as a composite indicator of living standards based on ownership of selected household assets, size of agricultural land, number of livestock, materials used for housing construction, ownership of improved water and sanitation facilities, and household possessions5. The wealth index values were calculated by summing up the scores of sixteen components. Ultimately, three categories (low, medium, and high) were generated by splitting the wealth index values into three equal classes.
Comparisons of mean hemoglobin level between and within the control and intervention groups were done using independent and paired sample t-tests (assuming equal variance), respectively. The analysis of the effect of the intervention was done using a Difference-In-Difference (DID) (percentage point change) non-parametric repeated two-samples test to compare outcomes between intervention and control groups before and after intervention. The changes in the dependent variable in the intervention group (from baseline to end line) were compared to the changes in the control group (from baseline to the endline). The intervention effect was measured by the odds ratio and 95% confidence level of the interaction term between study groups (intervention and control) and period of study (baseline and the endline) in the multivariate logistic regression model by adjusting the possible confounding variables. The Generalized Estimation Equation (GEE) was applied in addition to allow correlations of these repeated observations over time since data are collected on the same participants across successive points in time. A p < 0.05 was considered statistically significant.
Results
In the study, 99 pregnant women received nutrition education as well as IFAS, while 99 pregnant women received routine education only. Five pregnant women left the study. Among them, two participants could not be followed up, one shifted residence, and two had abortions (Fig. 1).
There was no significant difference between the intervention and control groups regarding age, parity, educational level, ethnicity, religion, occupation, family size, gravidity, parity, and socioeconomic level (Table 1).
At baseline, only 53.5% of the control group and 48.5% of the intervention group had a good knowledge level about anemia and IFAS. After intervention, more than three-fourths of the pregnant women (84.5%) in the intervention group had a good knowledge level on anemia and IFAS, compared to less than two-thirds (62.9%) in the control group (Table 2). The intervention had a net effect of 27.7% points (35–7.3) of improvement in IFA supplementation knowledge level, resulting in the statistical significance of the difference in difference (DID) between the two groups (p < 0.001).
The study also showed that the level of anemia was decreased by 20.6% points in the intervention group (from 27.8 to 7.2%) as compared to 9.4% points (from 27.1 to 17.7%) in the control group.
The intervention had a net effect of 11.2% points (20.6–9.4) reduction in the prevalence of anemia. Therefore, the statistical significance of the difference in difference (DID) between the two groups was < 0.001.
There was a significant change in hemoglobin level between intervention and control group after the intervention was implemented. The mean hemoglobin level within intervention group before and after intervention was (11.78 ± 1.33, 12.65 ± 1.26) (p < 0.001 (Table 3). The result showed that the intervention improves the mean hemoglobin level by 0.8 g/dL (Table 4).
After intervention, the proportion of adherence to the IFAS was 60% (n = 116). With regard to adherence within the groups, 79.4% (n = 77) in the intervention group and 40.6% (n = 39) in the control group and the intervention group were significantly higher than in the control group. In the intervention group, the proportion of adherence to the IFAS intake among participants increased by 45.6% points and was statistically different (P < 0⋅001). At the end of the study, the proportion of adherence to the IFAS also increased by 8.2% points in the control group but was not statistically different (P = 0.12). The difference in difference between the two groups of adherence to the IFAS intake was 37⋅4% and they were statistically significant (P < 0⋅001) (Table 5). At the endline, adherence between the groups did differ from the baseline (p = 0.12 vs. p < 0.001).
There was significant improvement in the levels of IFAS knowledge at the end line. The odds of being in compliance with IFAS at endline were 2.7 times higher than those at baseline (AOR = 3.9; 95% CI: 21.672, 4.825), adjusting for other factors (Table 6). Maternal educational status was significantly influenced prenatal IFA supplementation; as compared to women with no formal education, those in secondary and above education had 4 times increased odds of utilizing the supplementation (AOR = 4.076; 95%CI: (1.942, 8.556) (Table 5).
Discussion
The present study aimed to evaluate the effect of nutrition education and counseling, utilizing health belief model constructs and iron-folic acid supplementation, on the hemoglobin level and adherence to IFAs in pregnant women. The key findings were that the health belief model-based nutrition education and IFAS led to improved pregnant women’s knowledge about anemia and IFAS, hemoglobin levels, a drop in anemia proportion, and adherence to IFAS.
Reduced anemia prevalence has been reported in other studies that used nutrition education as an intervention29,30. A randomized control trial study conducted in Ghana reported parallel results, indicating a positive association between improved hemoglobin levels and nutrition education31. Similarly, a study on Indian pregnant women reported that individual counseling was found to improve hemoglobin levels in the intervention group as compared to the control32. In a study by Alaofe et al., the mean score of knowledge and hemoglobin level showed a significant increase after the intervention in the experimental group as compared to control group33. The possible reason for the drop in prevalence of anemia and/or improvement of hemoglobin levels might be that education about the consequences of anemia and the benefits of iron on pregnant women and fetus health might have encouraged women to comply with the nutrition advice in reducing anemia. Iron-folic acid supplementation may have also contributed to the reduction in the rate of anemia in the intervention group34,35.
A review of randomized control trials and quasi-experimental studies showed a substantial reduction of anemia in pregnant women when nutrition education and counseling were provided with nutritional supplements like micronutrient supplements compared to nutrition education alone21. For example, according to the Ethiopia Demographic and Health Survey (EDHS), < 11% took an IFAS for the recommended period (≥ 90); about 12% took 60–89 pills; more than one-third (35.7%) took < 60 pills, and around 42.2% did not take any iron tablets during their most recent pregnancy36. Thus, adherence to IFAS is still low in pregnant women in Ethiopia, indicating that Ethiopia is off-track to achieve the World Health Assembly (WHA) target of a 50% reduction of the prevalence of anemia by 202537. Integration of counseling and nutrition education into routine health extension programs may be considered potential public health interventions to reduce anemia among pregnant women in Ethiopia. Evidence has demonstrated that nutrition education and counseling that is targeted at maternal diet and supplement intakes during pregnancy, even when provided for a brief period of time, can improve multiple maternal and neonatal health outcomes21. However, most counseling done during ANC services tends to be general in the context of Ethiopia. Our finding suggests pregnant women who have good nutritional knowledge can have improved adherence to IFAS. Thus, nutrition education and counseling during ANC visits could improve maternal knowledge of IFAS.
In this study, the adherence to IFAS intake was 33.8% before the intervention and 79.4% after the intervention within the intervention group, compared with the 32.4 and 40.6% (before and after intervention) within the control group, and the average number of tablets taken in the intervention group was significantly higher than in the control group. This means there was an improvement in the proportion of women who consistently took the IFAS tablets as recommended. Therefore, targeted nutrition education, along with link to IFAS is one of the promising interventions that could improve the pregnancy and birth outcome. Similar results were reported by other studies conducted with the nutrition education and individual counseling in Nepal, Indonesia and India30,32,38. Studies conducted by Abdisa et al. and Berhane et al. showed that nutrition education and counseling during pregnancy can improve adherence to IFAS17,18. A study by Araban et al. also showed that nutritional education based on the Health Belief Model increased iron and folic acid intake in pregnant women39.
Furthermore, we assessed the behavior-related factors of maternal adherence to IFAS and showed a decrease in side effects reported at endline compared to baseline, especially in the intervention group. In addition, the study showed more awareness of the mitigation of IFAS side effects in the intervention group. The number of women who reported IFAS-related side effects in the intervention group dropped from 26 to 12% at the endline. This result can be explained by the fact that by providing ample information about the benefits of IFAs and the consequences of not doing so, there is a high possibility that the pregnant women perceived that the benefits of taking IFA tablets outweighed the side effects. Studies also reported that forgetfulness and side effects are one of the main factors contributing non-adherence to IFA tablet supplementation32,40. Other studies have shown that educating pregnant women on how to mitigate the side effects of IFAS often leads to higher adherence24,41. Therefore, it is highly recommended to make pregnant women aware of the possible side effects and how to mitigate them in order to improve adherence to IFAS as indicated elsewhere20,24.
The findings of the present study show that the odds of adherence to IFAS were 2.3 times higher among those women who received nutrition education than those who did not. This finding is in agreement with studies conducted in Kenya and Ethiopia, which resulted in improved adherence to IFAS among women who received education compared to the control group17,20,42. Additionally, primary and above maternal educational status was positively associated with adherence to IFAS. Consistent findings were reported by the study conducted in Senegal43, Iran44 and Ethiopia42. Maternal education could create opportunities for women to easily access information disseminated through health professionals and media about personal healthcare, IFAS, and its benefits. Moreover, pregnant women who have good knowledge and a positive attitude about IFAS were more likely to adhere to IFAS than women who had poor knowledge and a negative attitude towards IFAS. This might be due to the fact that knowledge helps a woman to have a good perception of the advantage of taking IFA tablets and the consequences of not taking the supplement during pregnancy. Studies conducted in India40, Kenya20 and Ethiopia45 have indicated a significant association between knowledge of IFAS and increased adherence to IFA tablets.
The present study has some limitations. Firstly, the sample size included in this study was smaller; therefore, the findings cannot be generalized to a wider population. Secondly, since only hemoglobin levels were measured, we did not assess iron deficiency, nutritional deficiency or inflammation anemia. Thirdly, pregnant women were assigned to either the control or intervention groups purposively. So, there was a chance of bias due to a lack of randomization.
Conclusion
Our study revealed that the provision of Health Belief Model-based nutrition education and counseling, along with IFA tablet supplementation, improved hemoglobin levels and adherence to IFAS intake among pregnant women. Nutrition education and counseling intervention strategies based on HBM constructs can improve adherence to folic acid intake and hemoglobin levels in pregnant women in primary health care settings in Ethiopia. Therefore, integration of theory-based nutrition education and counseling into routine antenatal care services in the primary health care systems is important to reduce the prevalence of anemia among women and achieve Sustainable Development Goal 2. A study that tests whether interventions grounded in theories of complex behavior change, that address other determinants of IFAS or adult educational theories are more effective than present nutrition education and counseling approaches is needed.
Data availability
All relevant data for this study are available upon reasonable request from the corresponding author.
Abbreviations
- IFAS:
-
iron-folic acid supplementation
- CG:
-
control group
- IG:
-
intervention group
- SD:
-
standard deviation
- HBM:
-
health belief model
References
-
Stevens, G. A. et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Heal. 1 (1), 16–25 (2013).
Google Scholar
-
Balarajan, Y., Ramakrishnan, U., Özaltin, E., Shankar, A. H. & Subramanian, S. V. Anaemia in low-income and middle-income countries. Lancet 378 (9809), 2123–2135 (2011).
Google Scholar
-
Benson, C. S. et al. The effect of iron deficiency and anaemia on women’s health. Anaesthesia 76, 84–95 (2021).
Google Scholar
-
Parks, S. et al. Maternal anaemia and maternal, fetal, and neonatal outcomes in a prospective cohort study in India and Pakistan. BJOG Int. J. Obstet. Gynaecol. 126 (6), 737–743 (2019).
Google Scholar
-
Central Statisctical Agency. Demographic and Health Survey. Vol. 1. (2016).
-
World Health Organization. Guideline: Daily iron and folic acid supplementation in pregnant women. World Heal Organ. 46, 323–329 (2012).
-
World Health Organization. Nutritional Anaemias: Tools for Effective Prevention [Internet]. World Health Organization. 1–83 p. (2017). Available from: https://iris.who.int/handle/10665/259425
-
Peña-Rosas, J. P., De-Regil, L. M., Garcia-Casal, M. N. & Dowswell, T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2015 (7), 1–527 (2015).
-
Imdad, A. & Bhutta, Z. A. Routine iron/folate supplementation during pregnancy: Effect on maternal anaemia and birth outcomes. Paediatr. Perinat. Epidemiol. 26 (SUPPL. 1), 168–177 (2012).
Google Scholar
-
Titaley, C. R., Dibley, M. J., Roberts, C. L. & Agho, K. Combined iron/folic acid supplements and malaria prophylaxis reduce neonatal mortality in 19 sub-Saharan African countries. Am J Clin Nutr. ;92(1):235–43. (2010). Available from: https://doi.org/10.3945/ajcn.2009.29093
-
Titaley, C. R., Dibley, M. J., Roberts, C. L., Hall, J. & Agho, K. Iron and folic acid supplements and reduced early neonatal deaths in Indonesia. Bull. World Health Organ. 88 (7), 500–508 (2010).
Google Scholar
-
Gebreamlak, B., Dadi, A. F. & Atnafu, A. High adherence to iron/folic acid supplementation during pregnancy time among antenatal and postnatal care attendant mothers in Governmental Health Centers in Akaki Kality Sub City, Addis Ababa, Ethiopia: hierarchical negative binomial poisson regression. PLoS One. 12 (1), 1–11 (2017).
Google Scholar
-
Digssie Gebremariam, A., Abebaw Tiruneh, S., Abebe Abate, B., Tadege Engidaw, M. & Tesfa Asnakew, D. Adherence to iron with folic acid supplementation and its associated factors among pregnant women attending antenatal care follow up at Debre Tabor General Hospital, Ethiopia, 2017. PLoS One. 14 (1), 1–10 (2019).
-
Edeo Berarti, A., Gebrie, M. & Beyene, B. Adherence to iron folic acid supplementation and associated factors among antenatal CARE attending women in Sire district primary health care units, South-East Ethiopia: A facility based cross-sectional study. Int J Africa Nurs Sci [Internet]. ;18(January):100526. (2023). Available from: https://doi.org/10.1016/j.ijans.2023.100526
-
Galloway, R. et al. Women’s perceptions of iron deficiency and anemia prevention and control in eight developing countries. Soc Sci Med. ;55(4):529–44. (2002). Available from: https://www.sciencedirect.com/science/article/pii/S027795360100185X
-
Nielsen, J. N., Gittelsohn, J., Anliker, J. & O’Brien, K. Interventions to Improve Diet and Weight Gain among Pregnant Adolescents and Recommendations for Future Research. J Am Diet Assoc. ;106(11):1825–40. (2006). Available from: https://doi.org/10.1016/j.jada.2006.08.007
-
Abdisa, D. K. et al. Effect of community based nutritional education on knowledge, attitude and compliance to IFA supplementation among pregnant women in rural areas of southwest Ethiopia: a quasi experimental study. BMC Public. Health. 23 (1), 1–10 (2023).
Google Scholar
-
Berhane, A. & Belachew, T. Effect of picture-based health education and counselling on knowledge and adherence to preconception Iron-folic acid supplementation among women planning to be pregnant in Eastern Ethiopia: a randomized controlled trial. J. Nutr. Sci. ;11. (2022).
-
Kavle, J. A. & Landry, M. Community-based distribution of iron-folic acid supplementation in low- and middle-income countries: a review of evidence and programme implications. Public. Health Nutr. 21 (2), 346–354 (2018).
Google Scholar
-
Kamau, M., Mirie, W., Kimani, S. & Mugoya, I. Effect of community based health education on knowledge and attitude towards iron and folic acid supplementation among pregnant women in Kiambu County, Kenya: a quasi experimental study. PLoS One. 14 (11), 1–21 (2019).
Google Scholar
-
Girard, A. W. & Olude, O. Nutrition education and counselling provided during pregnancy: effects on maternal, neonatal and child health outcomes. Paediatr. Perinat. Epidemiol. 26 (SUPPL. 1), 191–204 (2012).
Google Scholar
-
Wakwoya, E. B., Belachew, T. & Girma, T. Effect of intensive nutrition education and counseling on hemoglobin level of pregnant women in East Shoa zone, Ethiopia: randomized controlled trial. BMC Pregnancy Childbirth. ;23(1):1–11. (2023). Available from: https://doi.org/10.1186/s12884-023-05992-w
-
Mensur Reshid and Anchamo Anato. Community-based nutrition education and counselling provided during pregnancy: effects on knowledge and attitude towards iron-folic acid supplementation. J Nutr Sci. ;4(10):1–10. (2015). Available from: https://www.cambridge.org/core/services/aop-cambridge-core/content/view/3AB29B7E18369E99420867CBE28484F7/S2048679014000688a.pdf/div-class-title-a-randomised-double-blind-cross-over-study-investigating-the-prebiotic-effect-of-agave-fructans-in-healthy-huma
-
Gebremedhin, S., Samuel, A., Mamo, G., Moges, T. & Assefa, T. Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: a cross-sectional study. BMC Public. Health. 14 (1), 1–8 (2014).
Google Scholar
-
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switz World Heal Organ. ;1–6. (2011). Available from: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Haemoglobin+concentrations+for+the+diagnosis+of+anaemia+and+assessment+of+severity#1
-
Jones, C. L. et al. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 30(6), 566–576. https://doi.org/10.1080/10410236.2013.873363 (2015).
-
Federal ministry of health. Guidelines for the prevention and control of micronutrient deficiencies in Ethiopia Federal Ministry of Health. Guideline. (2020).
-
Bellg, A. J. et al. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations from the NIH Behavior Change ConsortiumVol. 23, : p. 443–451 (American Psychological Association, 2004). Health Psychology. Bellg, Albert J.: Appleton Heart Institute, 1818 North Meade Street, Appleton, WI, US, 54911, [email protected].
-
Wiafe, M. A., Apprey, C. & Annan, R. A. Nutrition Education Improves Knowledge of Iron and Iron-Rich Food Intake Practices among Young Adolescents: A Nonrandomized Controlled Trial. Int J Food Sci. ;2023. (2023).
-
Sunuwar, Sangroula, R. K. et al. Effect of nutrition education on hemoglobin level in pregnant women: a quasi- experimental study. ;1–12. (2019).
-
Otoo, G. & Adam, Y. Effect of Nutrition Education with an Emphasis on Consumption of Iron-Rich Foods on Hemoglobin levels of Pregnant Women in Ghana. FASEB J. ;30(S1):410.2-410.2. (2016). Available from: https://doi.org/10.1096/fasebj.30.1_supplement.410.2
-
Ramachandran, R. et al. Effect of individual nutrition education on perceptions of nutritional iron supplementation, adherence to iron – folic acid intake and Hb levels among a cohort of anemic South Indian pregnant women. J Matern Neonatal Med. ;36(1). (2023). Available from: https://doi.org/10.1080/14767058.2023.2183749
-
Alaofè, H., Zee, J., Dossa, R. & Brien, H. T. O. Education and improved iron intakes for treatment of mild iron-deficiency anemia in adolescent girls in southern Benin. Food Nutri. Bullet. 30(1), 24–36 (2009).
-
Bhutta, Z. A. et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 382 ()(9890), 452–477 (2013).
Google Scholar
-
Das, P. Can we eliminate nutritional anaemia in the near future? South East Asia. J. Public. Heal. 5 (1), 1–3 (2015).
Google Scholar
-
EPHI and ICF. Ethiopia Mini Demographic and Health Survey 2019: key Indicators [Internet]. Rockville, Maryland, USA: EPHI and ICF. 1–35 p. (2019). Available from: https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf
-
WHO. Comprehensive implementation plan on maternal, infant and young child nutrition. Glob Nutr Targets 2025. ;2012:12–3. (2012). Available from: www.who.int/nutrition/topics/nutrition_
-
Putri Nahrisah, R., Somrongthong, N. & Viriyautsahakul, Pramon Viwattanakulvanid, S. P. Effect of integrated pictorial handbook education and counseling on improving anemia status, knowledge, food intake, and iron tablet compliance among anemic pregnant women in Indonesia: a quasi-experimental study. J. Multidiscip Healthc. 13, 141–142 (2020).
Google Scholar
-
Araban, M., Baharzadeh, K. & Karimy, M. Nutrition modification aimed at enhancing dietary iron and folic acid intake: an application of health belief model in practice. Eur. J. Public. Health. 27 (2), 287–292 (2017).
Google Scholar
-
Lavanya, R. & Jayalakshmy, Sathish Rajaa, T. M. Universal health coverage – There is more to it than meets the eye. J Fam Med Prim Care. ;6(2):169–70. (2017). Available from: http://www.jfmpc.com/article.asp?issn=2249-4863;year=2017;volume=6;issue=1;spage=169;epage=170;aulast=Faizi
-
Nisar, Y., Bin, Alam, A., Aurangzeb, B. & Dibley, M. J. Perceptions of antenatal iron-folic acid supplements in urban and rural Pakistan: a qualitative study. ;1–12. (2014).
-
Sendeku, F. W., Azeze, G. G. & Fenta, S. L. Adherence to iron-folic acid supplementation among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 20 (1), 1–9 (2020).
Google Scholar
-
Niang, K. et al. Determinants of Iron consumption among pregnant women in Southern Senegal. Open. J. Obstet. Gynecol. 07 (01), 41–50 (2017).
Google Scholar
-
Siabani, S. et al. Determinants of Compliance With Iron and Folate Supplementation Among Pregnant Women in West Iran: A Population Based Cross-Sectional Study. J Fam Reprod Heal. ;12(4):197–203. (2018). Available from: http://www.ncbi.nlm.nih.gov/pubmed/31239847. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC6581656
-
Lencha, B. et al. Compliance to iron folic acid supplementation and its associated factors among pregnant women attending Antenatal clinic in Wondo district: a cross-sectional study. Sci Rep. ;13(1):1–8. (2023). Available from: https://doi.org/10.1038/s41598-023-44577-7
Acknowledgements
The authors thank all of the study participants, data collectors and supervisors who participated in the study, as well as the kind and cooperative staff of the health facilities and district’s administration, in southern Ethiopia.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
AA and MR conceptualized and designed the study and conducted statistical analysis, MR supervised the field data collection and AA and MR done interpretation and wrote the manuscript. AA and MR reviewed manuscript drafts. Both authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical considerations
Ethical clearance was obtained from Hawassa University Institutional Review Board before this study began (Ref. No. IRB/040/13). The purpose of the study was explained in a formal letter to district administration and permission obtained from authorities. The nature of the study was fully explained to the study participants and informed written consent was obtained from them before enrolling in the study. Emphasis on confidentiality and privacy were made clear at the time of consenting to participate and upheld throughout the study. No name appeared on the questionnaires so no participant identification with information could occur. Respondents were at liberty to discontinue from the study at any time without facing any adverse consequences. Information was kept confidential by restricted access and coding of questionnaires. While assessing anemia status, the result of the test was communicated immediately to each participant and if the pregnant woman was severely anemic, she was referred to the nearest health institution for treatment and follow-up. The trial for the study was retrospectively registered on Pan African Clinical Trials.gov with a registration number of PACTR202412578257739 on 11/12/2024. The study was reported following CONSORT 2010 statement (Fig. 1).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Reprints and permissions
About this article
Cite this article
Anato, A., Reshid, M. Effect of nutrition education and iron-folic acid supplementation on anemia among pregnant women in Ethiopia: a quasi-experimental study.
Sci Rep 15, 3556 (2025). https://doi.org/10.1038/s41598-025-87957-x
-
Received: 16 May 2024
-
Accepted: 23 January 2025
-
Published: 28 January 2025
-
DOI: https://doi.org/10.1038/s41598-025-87957-x
Keywords
- Nutrition education
- Pregnancy
- Hemoglobin
- Anemia
- Adherence
- IFAS