Pregnant women suffering from anemia, which affects approximately 38% of this population globally, now have hope as recent research conducted in Ethiopia indicates significant reductions in anemia rates due to comprehensive nutrition education and iron-folic acid supplementation.
The quasi-experimental study focused on pregnant women from Butajira, Ethiopia, where anemia prevalence has remained alarmingly high. Researchers implemented community-based nutrition education using the health belief model alongside the provision of iron-folic acid supplementation. Results showed a marked decrease in the proportion of anemia among the intervention group, dropping from 27.8% at baseline to just 7.2% after six weeks. Preliminary findings also suggested the odds of adherence to iron-folic acid supplements were 2.26 times higher among recipients of the nutrition education compared to those who received no such guidance.
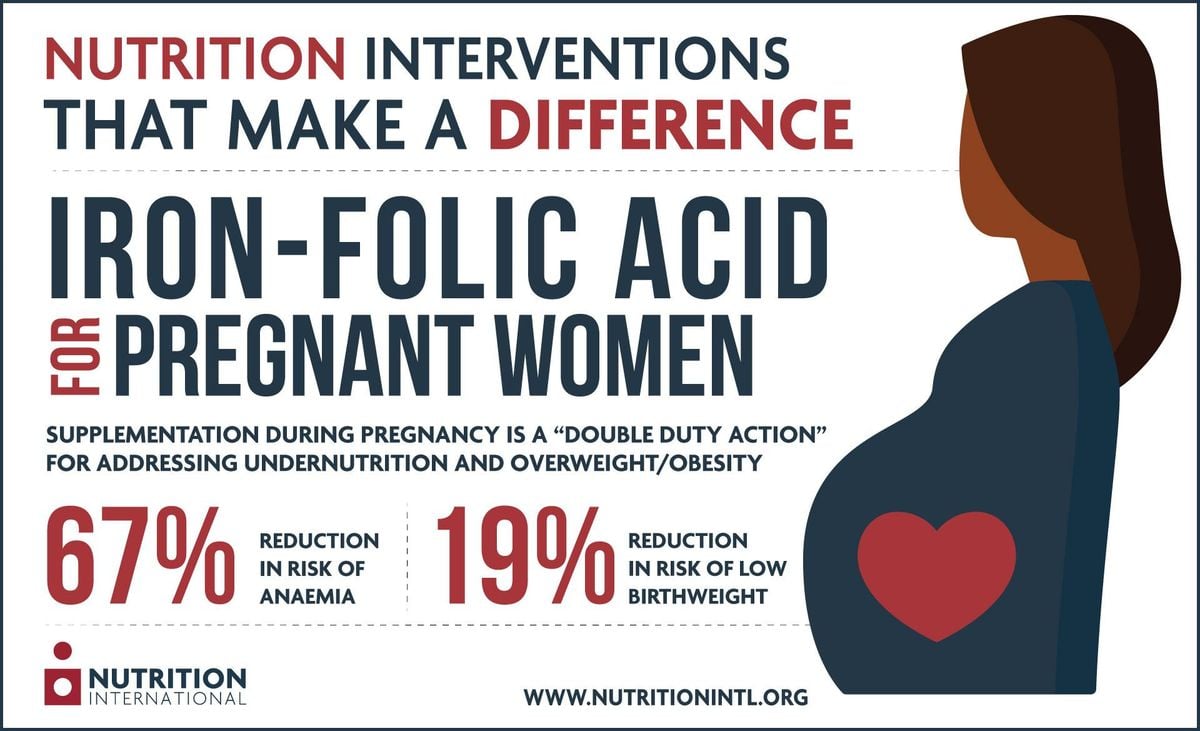
Despite efforts to address iron deficiency, the prevalence of anemia among pregnant women remained relatively unchanged over the last decade, highlighting the necessity for effective intervention strategies. The World Health Organization recommends 60 mg of iron and 0.4 mg of folic acid per day for pregnant women to mitigate risks associated with anemia, including low birth weight and maternal mortality. Yet, adherence to iron-folic acid supplementation has historically been low, primarily due to factors like socioeconomic challenges, lack of knowledge, and negative perceptions.
Participatory education sessions aimed at improving knowledge on the importance of iron and folic acid for maternal health were conducted among pregnant women, with data collection before and after the intervention. The study found significant enhancements not only in knowledge but also adherence to iron-folic acid supplements, showcasing the pivotal role of community-based education. This approach is particularly influential as conventional antenatal care often lacks structured nutrition education, undermining efforts to combat anemia.
Analysis of data taken before and after the study revealed the intervention group had considerably higher knowledge levels about the importance of iron and folate intake compared to the control group. Education led to improved awareness of the benefits of supplements with fewer reported side effects, indicating such programs may bolster adherence through informed engagement.
Looking forward, integrating such community-centric educational interventions within routine antenatal care could pave the way for reducing anemia prevalence effectively among pregnant women throughout Ethiopia and beyond. These findings present strong evidence for public health officials to adopt similar practices across other regions dealing with similar health challenges.
Research co-author A. Anato emphasized the importance of education about the benefits of iron intake stating: “Implementation of community-based nutrition education and counseling along with IFAS improved the hemoglobin level and adherence to IFAS among pregnant women”. The study sets a precedent for future programs aiming to address maternal health issues linked to nutritional inadequacy, presenting findings beneficial not only to the Ethiopian population but also within comparable contexts globally.