Kehoe L, Walton J, Flynn A. Nutritional challenges for older adults in Europe: current status and future directions. Proceedings of the Nutrition Society. 2019;78(2):221–33.
Google Scholar
Martins AD, et al. Effects of exercise programs on phase angle in older adults: A systematic review and meta-analysis. Arch Gerontol Geriatr. 2022;103: 104787.
Google Scholar
Ophey A, et al. Cognition in People Aged 80 Years and Older: Determinants and Predictors of Change from a Population-Based Representative Study in Germany. J Frailty Aging. 2023;12(3):189–97.
Google Scholar
Christensen K, et al. Ageing populations: the challenges ahead. The lancet. 2009;374(9696):1196–208.
Google Scholar
Konda S, Giri P. Prevalence of malnutrition and its determinants in an elderly people in South India. Int J Community Med Public Health. 2018;5(8):3570–6.
Google Scholar
Maseda A, et al. Health determinants of nutritional status in community-dwelling older population: the VERISAÚDE study. Public Health Nutr. 2016;19(12):2220–8.
Google Scholar
Sripongpunkul C, et al. Factors associated with unintentional weight loss among older adults in a geriatric outpatient clinic of university hospital. PLoS ONE. 2021;16(11): e0260233.
Google Scholar
Ferrari L, et al. Feasibility and effectiveness of a 6-month, home-based, resistance exercise delivered by a remote technological solution in healthy older adults. Arch Gerontol Geriatr. 2024;127: 105559.
Google Scholar
Maier AB, et al. Strengthening Muscle Health of Community-Dwelling Older Adults in Singapore: Evidence Towards Clinical Implementation. J Frailty Aging. 2023;12(4):258–66.
Google Scholar
Lorbergs A, et al. Nutrition and physical activity clinical practice guidelines for older adults living with frailty. J Frailty Aging. 2022;11(1):3–11.
Google Scholar
Mayo A, et al. Can an active lifestyle offset the relationship that poor lifestyle behaviours have on frailty? Arch Gerontol Geriatr. 2024;127: 105556.
Google Scholar
Amarya, S., K. Singh, and M. Sabharwal, Ageing process and physiological changes, in Gerontology. 2018. IntechOpen.
Saghafi-Asl M, et al. Geriatric nutritional risk index as a simple tool for assessment of malnutrition among geriatrics in Northwest of Iran: comparison with mini nutritional assessment. Aging Clin Exp Res. 2018;30:1117–25.
Google Scholar
Gall M, Harmer J, Wanstall H. Prescribing of oral nutritional supplements in Primary Care: can guidelines supported by education improve prescribing practice? Clin Nutr. 2001;20(6):511–5.
Google Scholar
Cramer JT, et al. Impacts of High-Protein Oral Nutritional Supplements Among Malnourished Men and Women with Sarcopenia: A Multicenter, Randomized, Double-Blinded, Controlled Trial. J Am Med Dir Assoc. 2016;17(11):1044–55.
Google Scholar
Elia M, et al. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in community and care home settings. Clin Nutr. 2016;35(1):125–37.
Google Scholar
Seguy D, et al. Compliance to oral nutritional supplementation decreases the risk of hospitalisation in malnourished older adults without extra health care cost: Prospective observational cohort study. Clin Nutr. 2020;39(6):1900–7.
Google Scholar
Hamirudin AH, Charlton K, Walton K. Outcomes related to nutrition screening in community living older adults: A systematic literature review. Arch Gerontol Geriatr. 2016;62:9–25.
Google Scholar
Poscia A, et al. Effectiveness of nutritional interventions addressed to elderly persons: umbrella systematic review with meta-analysis. Eur J Pub Health. 2018;28(2):275–83.
Google Scholar
Deutz NE, et al. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin Nutr. 2016;35(1):18–26.
Google Scholar
Deutz NE, et al. Reduced mortality risk in malnourished hospitalized older adult patients with COPD treated with a specialized oral nutritional supplement: sub-group analysis of the NOURISH study. Clin Nutr. 2021;40(3):1388–95.
Google Scholar
Stratton RJ, Hébuterne X, Elia M. A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev. 2013;12(4):884–97.
Google Scholar
McGowan L, et al. The impact of oral rehabilitation coupled with healthy dietary advice on the nutritional status of adults: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2020;60(13):2127–47.
Google Scholar
Wright J, Baldwin C. Oral nutritional support with or without exercise in the management of malnutrition in nutritionally vulnerable older people: A systematic review and meta-analysis. Clin Nutr. 2018;37(6):1879–91.
Google Scholar
Chew STH, et al. Impact of specialized oral nutritional supplement on clinical, nutritional, and functional outcomes: A randomized, placebo-controlled trial in community-dwelling older adults at risk of malnutrition. Clin Nutr. 2021;40(4):1879–92.
Google Scholar
Li M, et al. Effectiveness of oral nutritional supplements on older people with anorexia: A systematic review and meta-analysis of randomized controlled trials. Nutrients. 2021;13(3):1–24.
Google Scholar
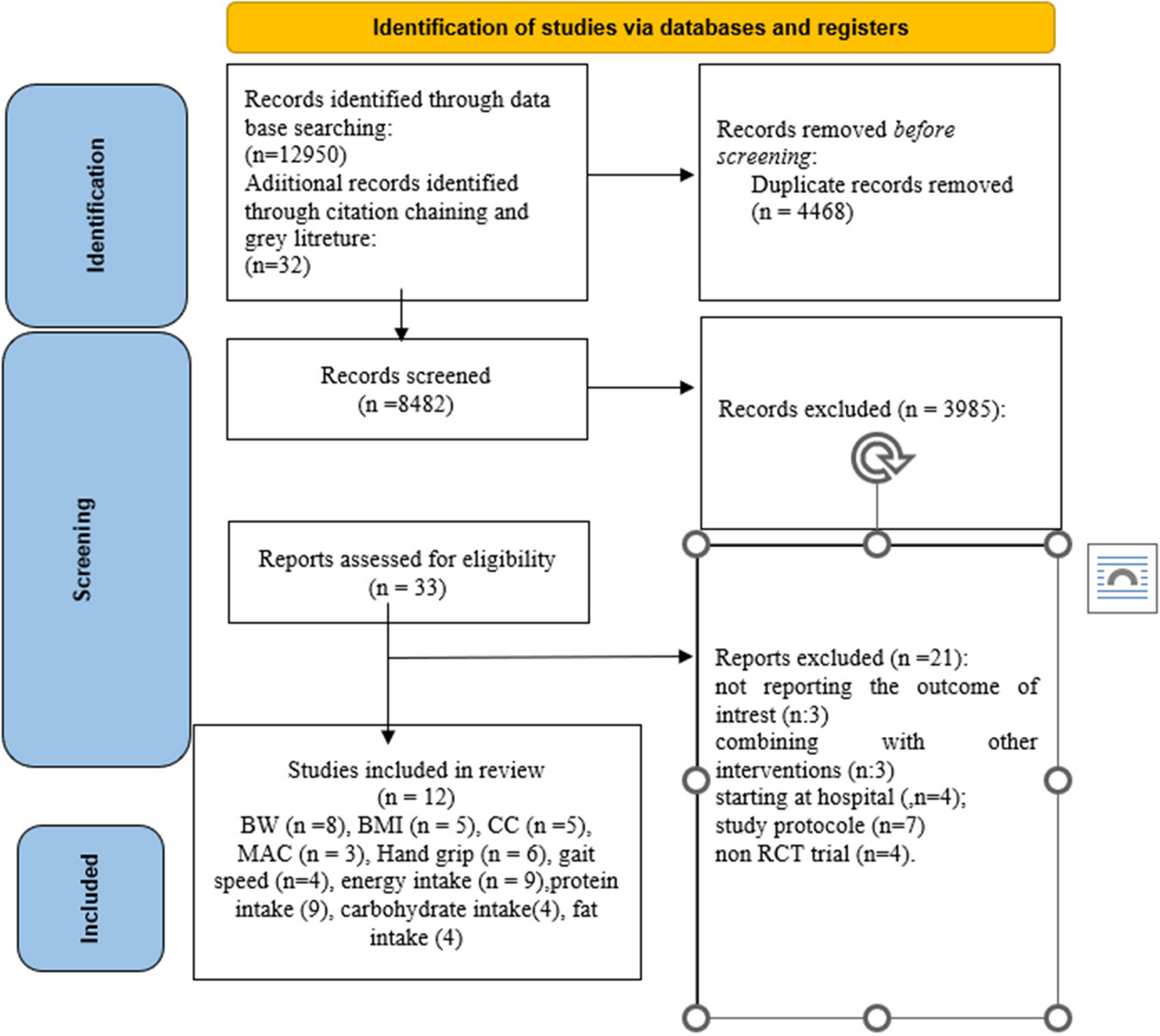
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94.
Google Scholar
Thomson KH, et al. Effectiveness and cost-effectiveness of oral nutritional supplements in frail older people who are malnourished or at risk of malnutrition: a systematic review and meta-analysis. The Lancet Healthy Longevity. 2022;3(10):e654–66.
Google Scholar
Higgins, J.P. and S. Green, Cochrane handbook for systematic reviews of interventions. 2008.
Blondal B, et al. HOMEFOOD randomised trial–Six-month nutrition therapy improves quality of life, self-rated health, cognitive function, and depression in older adults after hospital discharge. Clinical nutrition ESPEN. 2022;48:74–81.
Google Scholar
Bunout D, et al. The impact of nutritional supplementation and resistance training on the health functioning of free-living Chilean elders: results of 18 months of follow-up. J Nutr. 2001;131(9):2441S–2446S.
Google Scholar
Lipschitz DA, et al. Nutritional evaluation and supplementation of elderly subjects participating in a “meals on wheels” program. J Parenter Enter Nutr. 1985;9(3):343–7.
Google Scholar
Sugawara K, et al. Effects of nutritional supplementation combined with low-intensity exercise in malnourished patients with COPD. Respir Med. 2010;104(12):1883–9.
Google Scholar
Bonnefoy M, et al. Efficacy of a home-based intervention programme on the physical activity level and functional ability of older people using domestic services: a randomised study. J Nutr Health Aging. 2012;16:370–7.
Google Scholar
Woo J, et al. Randomized controlled trial of exercise and nutrition supplementation on physical and cognitive function in older Chinese adults aged 50 years and older. J Am Med Dir Assoc. 2020;21(3):395–403.
Google Scholar
Bruce D, et al. Nutritional supplements after hip fracture: poor compliance limits effectiveness. Clin Nutr. 2003;22(5):497–500.
Google Scholar
Neelemaat F, et al. Post-discharge nutritional support in malnourished elderly individuals improves functional limitations. J Am Med Dir Assoc. 2011;12(4):295–301.
Google Scholar
Gazzotti C, et al. Prevention of malnutrition in older people during and after hospitalisation: results from a randomised controlled clinical trial. Age Ageing. 2003;32(3):321–5.
Google Scholar
Terp R, et al. A nutritional intervention program improves the nutritional status of geriatric patients at nutritional risk—a randomized controlled trial. Clin Rehabil. 2018;32(7):930–41.
Google Scholar
Tieland M, et al. Protein supplementation improves physical performance in frail elderly people: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13(8):720–6.
Google Scholar
De Jong N, et al. Dietary supplements and physical exercise affecting bone and body composition in frail elderly persons. Am J Public Health. 2000;90(6):947.
Google Scholar
Lin, C.-C., et al., Effects of adequate dietary protein with whey protein, leucine, and vitamin D supplementation on sarcopenia in older adults: An open-label, parallel-group study. 2021.
Ng TP, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med. 2015;128(11):1225–1236. e1.
Google Scholar
Endevelt R, et al. Intensive dietary intervention by a dietitian as a case manager among community dwelling older adults: the EDIT study. J Nutr Health Aging. 2011;15:624–30.
Google Scholar
Cederholm T, Hellström K. Reversibility of protein-energy malnutrition in agroup of chronically-ill elderly outpatients. Clin Nutr. 1995;14(2):81–7.
Google Scholar
Faxen-Irving G, et al. The effect of nutritional intervention in elderly subjects residing in group-living for the demented. Eur J Clin Nutr. 2002;56(3):221–7.
Google Scholar
Zhang H, et al. The effect of oral nutritional supplements on the nutritional status of community elderly people with malnutrition or risk of malnutrition. Asia Pac J Clin Nutr. 2021;30(3):415–23.
Google Scholar
Arnaud-Battandier F, et al. Use of oral supplements in malnourished elderly patients living in the community: a pharmaco-economic study. Clin Nutr. 2004;23(5):1096–103.
Google Scholar
Smith TR, et al., Ready-Made Oral Nutritional Supplements Improve Nutritional Outcomes and Reduce Health Care Use-A Randomised Trial in Older Malnourished People in Primary Care. Nutrients. 2020;12(2).
Assantachai P, et al. The benefits of a novel chicken-based oral nutritional supplement for older adults: A double-blind randomized controlled trial. Asia Pac J Clin Nutr. 2020;29(4):743–50.
Google Scholar
Xie H, et al. Nutrition education with or without oral nutrition supplements has contrasting effects on nutrition status in older adults: A randomized controlled study. Nutr Clin Pract. 2023;38(1):138–47.
Google Scholar
Yeung SSY, JSW Lee, and T. Kwok. A Nutritionally Complete Oral Nutritional Supplement Powder Improved Nutritional Outcomes in Free-Living Adults at Risk of Malnutrition: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19(18).
Edington J, et al. A prospective randomised controlled trial of nutritional supplementation in malnourished elderly in the community: clinical and health economic outcomes. Clin Nutr. 2004;23(2):195–204.
Google Scholar
van de Bool C, et al. A randomized clinical trial investigating the efficacy of targeted nutrition as adjunct to exercise training in COPD. J Cachexia Sarcopenia Muscle. 2017;8(5):748–58.
Google Scholar
Wouters-Wesseling W, et al. The effect of a liquid nutrition supplement on body composition and physical functioning in elderly people. Clin Nutr. 2003;22(4):371–7.
Google Scholar
Payette H, et al. Benefits of nutritional supplementation in free-living, frail, undernourished elderly people: A prospective randomized community trial. J Am Diet Assoc. 2002;102(8):1088–95.
Google Scholar
Graydonald K, Payette H, Boutier V. RANDOMIZED CLINICAL-TRIAL OF NUTRITIONAL SUPPLEMENTATION SHOWS LITTLE EFFECT ON FUNCTIONAL STATUS AMONG FREE-LIVING FRAIL ELDERLY. J Nutr. 1995;125(12):2965–71.
Google Scholar
Krondl M, et al. Subjectively healthy elderly consuming a liquid nutrition supplement maintained body mass index and improved same nutritional parameters and perceived well-being. J Am Diet Assoc. 1999;99(12):1542–8.
Google Scholar
Kim CO, Lee KR. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: A community-based randomized controlled study. Journals of Gerontology – Series A Biological Sciences and Medical Sciences. 2013;68(3):309–16.
Google Scholar
Zhu L-Y, et al. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019;48(2):220–8.
Google Scholar
Multidisciplinary, three-dimensional and individualized comprehensive treatment for severe/critical COVID-19. Liver Res. 2020;4(3):109–117.
Smith TR, et al. Ready-made oral nutritional supplements improve nutritional outcomes and reduce health care use—a randomised trial in older malnourished people in primary care. Nutrients. 2020;12(2).
Giezenaar, C., et al., Ageing Is Associated with Decreases in Appetite and Energy Intake–A Meta-Analysis in Healthy Adults. Nutrients. 2016;8(1).
Johnson KO, et al. Differences in circulating appetite-related hormone concentrations between younger and older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32(7):1233–44.
Google Scholar
Perna S, et al. Are the therapeutic strategies in anorexia of ageing effective on nutritional status? A systematic review with meta-analysis. J Hum Nutr Diet. 2019;32(1):128–38.
Google Scholar
Li M, et al. Effectiveness of oral nutritional supplements on older people with anorexia: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2021;13(3):835.
Google Scholar
Li M, et al. Effectiveness of Oral Nutritional Supplements on Older People with Anorexia: a Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2021;13(3).
Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012;11(2):278–96.
Google Scholar
Allen VJ, Methven L, Gosney MA. Use of nutritional complete supplements in older adults with dementia: systematic review and meta-analysis of clinical outcomes. Clin Nutr. 2013;32(6):950–7.
Google Scholar
Reinders I, et al. Effectiveness of nutritional interventions in older adults at risk of malnutrition across different health care settings: Pooled analyses of individual participant data from nine randomized controlled trials. Clin Nutr. 2019;38(4):1797–806.
Google Scholar
Correa-Pérez A, et al. Efficacy of non-pharmacological interventions to treat malnutrition in older persons: A systematic review and meta-analysis. The SENATOR project ONTOP series and MaNuEL knowledge hub project. Ageing Res Rev. 2019;49:27–48.
Google Scholar
White JV, et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730–8.
Google Scholar
Wei J, et al. The association between low calf circumference and mortality: a systematic review and meta-analysis. European geriatric medicine. 2022;13(3):597–609.
Google Scholar
Chou MY, et al. Role of gait speed and grip strength in predicting 10-year cognitive decline among community-dwelling older people. BMC Geriatr. 2019;19(1):186.
Google Scholar
van Wijngaarden JP, et al. Effects of Nutritional Interventions on Nutritional and Functional Outcomes in Geriatric Rehabilitation Patients: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2020;21(9):1207–1215.e9.
Google Scholar
Veronese N, et al. Effect of nutritional supplementations on physical performance and muscle strength parameters in older people: A systematic review and meta-analysis. Ageing Res Rev. 2019;51:48–54.
Google Scholar
Cox NJ, et al. New horizons in appetite and the anorexia of ageing. Age Ageing. 2020;49(4):526–34.
Google Scholar
Cox NJ, et al. Older individual’s perceptions of appetite, its loss, influencing factors and adaptions to poor appetite. A qualitative study Appetite. 2021;167: 105609.
Landi F, et al. Anorexia of Aging: Risk Factors, Consequences, and Potential Treatments. Nutrients. 2016;8(2):69.
Google Scholar
Soenen S, Chapman IM. Body weight, anorexia, and undernutrition in older people. J Am Med Dir Assoc. 2013;14(9):642–8.
Google Scholar
Van Wymelbeke V, et al. An innovative brioche enriched in protein and energy improves the nutritional status of malnourished nursing home residents compared to oral nutritional supplement and usual breakfast: FARINE+ project. Clin Nutr ESPEN. 2016;15:93–100.
Google Scholar
Chapman IM. Weight loss in older persons. Med Clin North Am. 2011;95(3):579–93. xi.
Google Scholar
Chang M, et al. A poor appetite or ability to eat and its association with physical function amongst community-dwelling older adults: age, gene/environment susceptibility-Reykjavik study. Eur J Ageing. 2021;18:405–15.
Google Scholar
Elia M, et al. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr. 2016;35(2):370–80.
Google Scholar
Ryan M, et al. Oral supplements differing in fat and carbohydrate content: effect on the appetite and food intake of undernourished elderly patients. Clin Nutr. 2004;23(4):683–9.
Google Scholar
Parsons EL, et al. Oral nutritional supplements in a randomised trial are more effective than dietary advice at improving quality of life in malnourished care home residents. Clin Nutr. 2017;36(1):134–42.
Google Scholar
Hubbard GP, et al. A systematic review of compliance to oral nutritional supplements. Clin Nutr. 2012;31(3):293–312.
Google Scholar