Abstract
An abrupt outbreak of COVID-19 caused enormous global concerns. Although all countries around the world are severely affected, developing Asian countries faced more difficulties due to their low per capita GDP. The temperature was considered a leading variable in spreading viral diseases, including COVID-19. The present study aimed to assess the relationship between temperature and the spread of COVID-19, with a focus on developing Asian countries. In a few Asian countries, COVID-19 spread rapidly in the summer, while in some countries, there is an increase in winter. A linear correlation was developed between COVID-19 cases/deaths and temperature for the selected countries, which were very weak. A coefficient of determination of 0.334 and 0.365 was observed between cases and average monthly max/min temperatures. A correlation of R2 = 0.307 and 0.382 was found between deaths and average max/min monthly temperatures, respectively. There is no scientific reason to assume that COVID-19 is more dominant at low than high temperatures. Therefore, it is believed that the results may be helpful for the health department and decision-makers to understand the fast spread of COVID-19.
Introduction
Pandemic diseases have proved to be the most distressing in the history of mankind. For instance, the black death pandemic affected one-third of the population of Europe1,2,3, and the Spanish flu casualties more human beings than the entire victims of the first world war4,5,6,7. Recently, an abrupt epidemic outbreak of COVID-19 disease in 20198 has caused enormous global concerns within the scientific community and healthcare officials8,9,10. COVID-19 disease results from severe acute respiratory syndrome (SARS-CoV) and is usually transmitted through human droplets produced by coughing, sneezing, or talking11. More than 77.04 million people have been affected worldwide due to this outbreak (https://covid19.who.int/). These numbers are increasing exponentially daily, with the worst-case scenarios observed in the USA, India, Brazil, the UK, Italy, etc.
The outbreak of COVID-19 led to the disruption of the global economy12. Global per capita GDP fell by 4% on average13. This pandemic also affected the quality This pandemic also affected the sustainability of life was also impacted by this pandemic14. The impact of COVID-19 on GDP was also investigated by15 which showed that the average per capita GDP decreases due to the COVID-19 outbreak. Although all countries across the globe are severely affected by the COVID-19 pandemic, developing Asian countries face more difficulties due to their low per capita GDP, fewer healthcare facilities, and large population16. The COVID-19 pandemic has slowed down the GDP, along with major economic indicators. In Pakistan, tens of millions of people lost their jobs.
Moreover, this pandemic significantly affects Bangladesh’s population, and the 0.89 million population is at job risk. In Afghanistan, the people faced food insincerity, the country is still struggling from economic recession17. Nepal’s tourist industry was also affected due to this pandemic18. India’s economy is also affected; its growth rate dropped below 3.1%19.
Asian countries, particularly Afghanistan, Yemen, Syria, Nepal, Tajikistan, Kyrgyzstan, Cambodia, Bangladesh, Myanmar, and Pakistan, have very low per capita GDP and are one of the world’s poorest regions. About one-third of the world’s population lives in this region. Before the outbreak of this pandemic, people in these countries were moderately or severely food insecure and lived below the poverty line16,20,21 as most populated cities in the world like Mumbai, Delhi, Karachi, and Dhaka lie in these regions. The rapid increase in COVID-19 cases has affected the economy of these countries badly, and this situation is likely to increase further in the future22.
Human beings are already facing global challenges of water scarcity and climate change and are coming under the threat of the COVID-19 pandemic23,24. Several regions in Asia are experiencing climatic change, e.g., floods in Bangladesh and India, heavy rainfall events in Nepal, and receding water tables in Pakistan and India25. These climatic events have caused an exponential increase in the associated damage. Different studies were conducted to study the impact of meteorological conditions, i.e., relative humidity, sunshine hours, and temperature, on the spread of COVID-1926,27,28,29. These studies showed that high humidity can increase the spread of COVID-19, while some studies showed that low temperature resulted in the fast transmission of COVID-19. Also, the city’s lockdown resulted in improved air quality30.
According to most previous studies, climatic conditions, particularly temperature, were considered the leading variable in the spread of viral diseases, including COVID-19 worldwide31,32,33,34,35. Different studies have been conducted to assess the impact of temperature on the spread and outbreak of COVID-1936,37,38,39; however, the relationship between temperature in Asian countries and the COVID-19 pandemic is yet to be understood. Asian countries with low per capita GDP were selected, as these countries were already under stress due to low per capita GDP. There is a need to develop a prediction system for the COVID-19 pandemic30. Therefore, the present study aimed to assess the relationship between temperature and the spread of COVID-19, focusing on developing Asian countries. The results of this research may help better understand the linkages between two global crises of climate change and COVID-19, and address the challenges associated with it for sustainable economic development.
Materials and methods
Study area
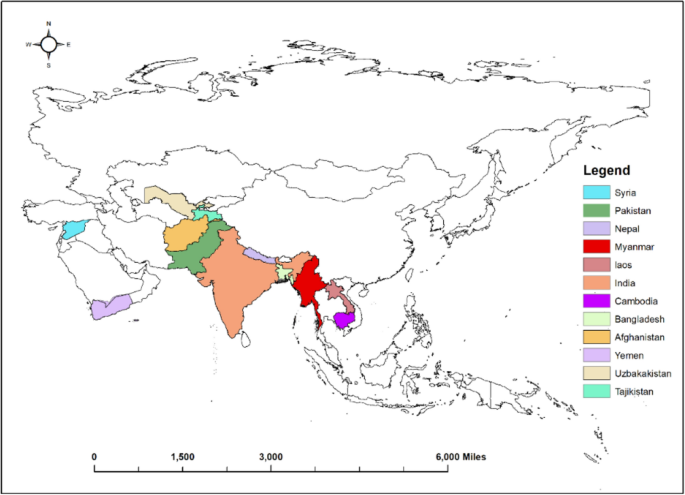
The study envisaged twelve (12) countries (Fig. 1), including West Asian countries, i.e., Syria and Yemen; South Asian countries, i.e., Afghanistan, Nepal, Bangladesh, Pakistan, and India; Central Asian countries, i.e., Tajikistan, Uzbekistan, and Southeast Asian countries, i.e., Cambodia, Myanmar, and Laos. The variations in the mean annual temperatures of these countries are presented in Fig. 2.

Map of the study area (Software used: ArcGIS Pro).

Average annual temperatures of countries.
Data collection
Data of COVID-19 cases was obtained from COVID-19 source data40. Average monthly temperature data was obtained from41. The countries for the study were selected based on nominal per capita GDP in USD. The GDP of developing Asian countries in the study area is shown in Table 1. These countries were divided into two groups based on low and high temperatures observed during the year. The first group contains six (06) countries with low temperature, i.e., Syria, Yemen, Afghanistan, Nepal, Tajikistan, and Uzbekistan. In contrast, group two contains countries with high temperatures, i.e., Pakistan, India, Bangladesh, Cambodia, Laos, and Myanmar.
The graphs of total cases and deaths per month were plotted with an average monthly temperature of COVID-19 reported cases for each low-GDP Asian country, as shown in Fig. 3. Average monthly temperature data was plotted on the secondary axis.


Total reported cases and deaths per month (in Thousands) with averaged monthly temperature.
Statistical analysis
The coefficient of determination (R2) was calculated to analyze the association of regional climatological parameters (averaged monthly maximum and minimum temperature) with the total monthly reported COVID-19 cases and total monthly deaths. The coefficient of determination (R2) showed vast variations for different data sets. Regression analysis was also applied to evaluate the correlation of reported cases and deaths for the summer and winter seasons. In the summer, months from March to August were considered, while the winter season includes the months from September to February. Correlation between reported cases and deaths was developed for countries where there is a trend of increase in reported cases and deaths during low temperatures, and countries with more reported cases and deaths during high temperatures both for the summer and winter seasons.
Results and discussion
The data on COVID-19 cases reported in selected Asian countries showed different trends for different regions. Few countries like Syria, Nepal, Myanmar, and Laos showed an increase in COVID-19 cases and deaths during the winter, while in some countries like Yemen, Tajikistan, Bangladesh, Uzbekistan, and India, a trend of increase in reported deaths and cases was observed in the summer. In Afghanistan, Pakistan, and Cambodia, an increase in reported cases and deaths during peak summer (June and July) and winter (November and December) was observed.
The countries found to be more sensitive to the winter season are Syria, Nepal, Myanmar, and Laos. In Syria, there were a maximum of 27.314 cases per million population, with a death rate of 1.943 per million population during the summer (average temperature 28 °C) whereas a significant increase during winter season 123.367 and 202.678 cases per million with 7.37 and 16.799 deaths per million population were observed during November and December with an average temperature of 12.6 °C and 7.65 °C, respectively. In Nepal, cases, and deaths per million population during the winter (14.65 °C) were almost six times higher than the reported cases and deaths during the summer (23.6 °C). Reported cases and deaths in Myanmar during the winter were disastrous. A significant increase in deaths and reported cases was observed during winter. An increasing trend in reported cases in Laos was not devastating. However, an increase in reported cases was observed in the winter during November (21.2 °C).
An increase in reported COVID-19 cases and deaths per million population during the summer season was observed in Yemen, Tajikistan, Bangladesh, Uzbekistan, and India. The reported cases and deaths in Yemen and Tajikistan during May, June, and July showed a significantly increasing trend compared to the reported cases and deaths during winter. In Bangladesh, there was an increase in COVID-19 cases and deaths during June, July, and August (average temperature 28.9 °C), which continued to decline in winter (20.1 °C). In Uzbekistan and India, significant cases and deaths were reported during the peak summer season (29.25 °C), with a decrease in the winter season.
Pakistan, Afghanistan, and Cambodia showed different trends from other countries. There was an increase in COVID-19 cases and deaths during peak summer and peak winter periods. In Afghanistan, the number of cases and deaths rises during May, June, and July, which decreases from August to October. However, an increase in cases and deaths was observed during the peak winter period. The same trend was observed in Pakistan, with a significant increase during the peak summer (June and July) and in the peak winter (November and December). In Cambodia, the highest reported cases were in the peak summer period (27.85 °C) and peak winter periods during November and December.
A linear correlation was developed between COVID-19 cases/ deaths and maximum/ minimum temperature for all countries, which were found to be very weak. A correlation of R2 = 0.334 and 0.365 between reported cases and mean maximum and mean minimum monthly temperature, respectively. A correlation of R2 = 0.307 and 0.382 was found between reported deaths and mean maximum and mean minimum monthly temperatures, respectively, as shown in Fig. 4.

Correlation between (a,b) max/min temperature and Cases per million population (c,d) max/min temperature and deaths per million population.
Moreover, a linear correlation was developed between reported cases and deaths per million population for the countries, showing an increase in COVID-19 cases during the summer, winter, and peak summer, and winter seasons with the help of the coefficient of determination model. Reported cases in Syria, Nepal, Myanmar, and Laos showed a correlation of 0.5375 and 0.846 with deaths during the winter and summer seasons, respectively. However, in Yemen, Tajikistan, Bangladesh, Uzbekistan, and India, a correlation of 0.98 and 0.7736 was found between cases and deaths during the winter and summer, respectively. The correlation of 0.5683 and 0.9164 was determined during the winter and summer seasons for all the countries combined, as shown in Fig. 5.

Correlation between deaths vs cases per million population during winter and summer season for (a,b) Countries showing an increase in COVID-19 during winter season (c,d) Countries showing an increase in COVID-19 during summer season (e,f) all countries combined.
The above results showed that the COVID-19 outbreak showed different trends during the summer and winter seasons. Some countries have increased COVID-19 cases during the summer, while others have a rapid outbreak during the winter. The linear correlation between maximum/minimum temperature and cases is 0.334–0.365, which is weak and shows no correlation between temperature and cases. A weak correlation between maximum/minimum temperature and deaths can also be observed. This correlation is not sufficient to prove the association of COVID-19 with temperature.
Population density can be a factor in the spread of COVID-19 in countries like India and Bangladesh. Pakistan and Nepal. Moreover, fewer healthcare facilities and improper lockdowns in developing countries, particularly Afghanistan, Laos, and Myanmar, are significant factors in the COVID-19 outbreak. The increase in cases and deaths was also observed in those months where COVID-19 SOPs were not properly followed.
The above discussion is supported by the fast spread of the novel COVID-19 MERS-CoV in Riyadh during the peak summer season despite high temperatures43; however, few studies showed negative relationships between temperature and COVID-19 cases44. Jahangiry et al.45 also concluded that there is no relationship between COVID-19 cases and the temperature.
Conclusions
This study investigated the effect of temperature on the spread of COVID-19 in low per capita GDP Asian countries. Few countries exhibited a fast spread of COVID-19 during the summer, and the rest showed an increase during the winter. The results indicated that there is no evidence that the number of people affected with COVID-19 depends on the variations in temperature in different regions. Therefore, no scientific reason was found to assume that COVID-19 is dominant at lower temperatures than the high temperature for these countries. The fast spread of COVID-19 at high and low temperatures may depend on the different variants of the virus, population density, living styles, etc.
This study suggested that proper management, such as social distancing and hand washing, may also slow down the spread of the COVID-19 virus. The results of this study may be helpful for the health department and decision-makers to understand the fast pace of COVID-Declarations.
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- GDP:
-
Gross domestic product
- SARS-CoV:
-
Severe Acute Respiratory Syndrome Coronavirus
- USD:
-
United States Dollar
References
-
Green, M. H. How a microbe becomes a pandemic: A new story of the Black Death. Lancet Microbe 1, e311–e312 (2020).
Google Scholar
-
Keilman, L. J. Seasonal influenza (Flu). Nurs. Clin. North Am. 54, 227–243 (2019).
Google Scholar
-
Bos, K. I. et al. A draft genome of Yersinia pestis from victims of the Black Death. Nature 478, 506–510 (2011).
Google Scholar
-
Djalante, R. et al. Review and analysis of current responses to COVID-19 in Indonesia: Period of January to March 2020. Progress Disast. Sci. 6, 100091 (2020).
Google Scholar
-
Gould, E. Emerging viruses and the significance of climate change. Clin. Microbiol. Infect. 15, 503 (2009).
Google Scholar
-
Malik, S., Hussain, S. & Waqas, M. S. effect of water quality and different meals on growth of Catla catla and Labeo rohita. Big Data Water Resour. Eng. 1, 04–08 (2020).
Google Scholar
-
Kandel, N., Chungong, S., Omaar, A. & Xing, J. Health security capacities in the context of COVID-19 outbreak: An analysis of International Health Regulations annual report data from 182 countries. Lancet 395, 1047–1053 (2020).
Google Scholar
-
WHO. Country & technical guidance-coronavirus disease. COVID-19. (2019).
-
Chaudhry, A. K. & Sachdeva, P. Coronavirus disease 2019 (COVID-19): A new challenge in untreated wastewater. Can. J. Civ. Eng. 47, 1005–1009 (2020).
Google Scholar
-
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Google Scholar
-
Shang, Y., Tao, Y., Dong, J., He, F. & Tu, J. Deposition features of inhaled viral droplets may lead to rapid secondary transmission of COVID-19. J. Aerosol. Sci. 154, 105745 (2021).
Google Scholar
-
Huang, J. et al. The oscillation-outbreaks characteristic of the COVID-19 pandemic. Natl. Sci. Rev. 8, 20 (2021).
Google Scholar
-
Mou, J. Research on the impact of COVID19 on global economy. IOP Conf. Ser. Earth Environ. Sci. 546, 032043 (2020).
Google Scholar
-
El Keshky, M. E. S., Basyouni, S. S. & Al Sabban, A. M. Getting through COVID-19: The Pandemic’s impact on the psychology of sustainability, quality of life, and the global economy—a systematic review. Front. Psychol. 11, 25 (2020).
Google Scholar
-
Beckman, J., Baquedano, F. & Countryman, A. The impacts of COVID-19 on GDP, food prices, and food security. Q Open 1, 25 (2021).
Google Scholar
-
Rasul, G. Twin challenges of COVID-19 pandemic and climate change for agriculture and food security in South Asia. Environ. Challenges 2, 100027 (2021).
Google Scholar
-
Islam, Z. et al. Food security, conflict, and COVID-19: Perspective from Afghanistan. Am. J. Trop. Med. Hyg. 106, 21–24 (2022).
Google Scholar
-
Islam, M., Jannat, A., AlRafi, D. A. & Aruga, K. Potential economic impacts of the COVID-19 pandemic on South Asian economies: A review. World 1, 283–299 (2020).
Google Scholar
-
MSPI. Ministry of Statistics and Programme Implementation (2020).
-
FAO. Responding to the Impact of the COVID-19 Outbreak on Food Value Chains Through Efficient Logistics (FAO, 2020). https://doi.org/10.4060/ca8466en
Google Scholar
-
UNICEF. Water, Sanitation, Hygiene, and Waste Management for the COVID-19 Virus: Interim Guidance (2020).
-
Sumner, A., Hoy, C. & Ortiz-Juarez, E. Estimates of the Impact of COVID-19 on Global Poverty Vol. 2020 (UNU-WIDER, 2020).
Google Scholar
-
Yokomatsu, M. et al. A multi-sector multi-region economic growth model of drought and the value of water: A case study in Pakistan. Int. J. Disast. Risk Reduct. 43, 101368 (2020).
Google Scholar
-
Iqbal, M. M., Shoaib, M., Farid, H. U. & Lee, J. L. Assessment of water quality profile using numerical modeling approach in major climate classes of Asia. Int. J. Environ. Res. Public Health 15, 2258 (2018).
Google Scholar
-
IPCC. AR4 Climate Change 2007: The Physical Science Basis (2007).
-
Hridoy, A.-E.E., Mohiman, A., Tusher, S. S. H., Nowraj, S. Z. A. & Rahman, M. A. Impact of meteorological parameters on COVID-19 transmission in Bangladesh: A spatiotemporal approach. Theor. Appl. Climatol. 144, 273–285 (2021).
Google Scholar
-
Sarkodie, S. A. & Owusu, P. A. Impact of meteorological factors on COVID-19 pandemic: Evidence from top 20 countries with confirmed cases. Environ. Res. 191, 110101 (2020).
Google Scholar
-
Bochenek, B. et al. Impact of meteorological conditions on the dynamics of the COVID-19 pandemic in Poland. Int. J. Environ. Res. Public Health 18, 3951 (2021).
Google Scholar
-
Huang, Z. et al. Optimal temperature zone for the dispersal of COVID-19. Sci. Total Environ. 736, 139487 (2020).
Google Scholar
-
Huang, J. et al. Global prediction system for COVID-19 pandemic. Sci. Bull. (Beijing) 65, 1884–1887 (2020).
Google Scholar
-
Liang, L. & Gong, P. Climate change and human infectious diseases: A synthesis of research findings from global and spatio-temporal perspectives. Environ. Int. 103, 99–108 (2017).
Google Scholar
-
Bourdrel, T., Bind, M.-A., Béjot, Y., Morel, O. & Argacha, J.-F. Cardiovascular effects of air pollution. Arch. Cardiovasc. Dis. 110, 634–642 (2017).
Google Scholar
-
Wu, X., Lu, Y., Zhou, S., Chen, L. & Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 86, 14–23 (2016).
Google Scholar
-
Lipfert, F. W. Long-term associations of morbidity with air pollution: A catalog and synthesis. J. Air Waste Manage. Assoc. 68, 12–28 (2018).
Google Scholar
-
Lee, B.-J., Kim, B. & Lee, K. Air pollution exposure and cardiovascular disease. Toxicol. Res. 30, 71–75 (2014).
Google Scholar
-
Yamasaki, L., Murayama, H. & Hashizume, M. The impact of temperature on the transmissibility and virulence of COVID-19 in Tokyo, Japan. Sci. Rep. 11, 24477 (2021).
Google Scholar
-
Yang, H.-Y. & Lee, J. K. W. The impact of temperature on the risk of COVID-19: A multinational study. Int. J. Environ. Res. Public Health 18, 4052 (2021).
Google Scholar
-
Sasikumar, K., Nath, D., Nath, R. & Chen, W. Impact of extreme hot climate on COVID-19 outbreak in India. Geohealth 4, 25 (2020).
Google Scholar
-
Ganslmeier, M., Furceri, D. & Ostry, J. D. The impact of weather on COVID-19 pandemic. Sci. Rep. 11, 22027 (2021).
Google Scholar
-
Ritchie, H. Coronavirus Source Data. https://ourworldindata.org/coronavirus-source-data (2021).
-
CDCW. Climate Data. https://en.climate-data.org/asia/ (2020).
-
IMF. World Economic Outlook Databases. (2020).
-
Altamimi, A. & Ahmed, A. E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. J. Infect. Public Health 13, 704–708 (2020).
Google Scholar
-
Abduljalil, J. M. & Abduljalil, B. M. Epidemiology, genome, and clinical features of the pandemic SARS-CoV-2: A recent view. New Microbes New Infect. 35, 100672 (2020).
Google Scholar
-
Jahangiry, L. et al. Risk perception related to COVID-19 among the Iranian general population: An application of the extended parallel process model. BMC Public Health 20, 1571 (2020).
Google Scholar
Author information
Authors and Affiliations
Contributions
F.U.H.: conceptualization, methodology, investigation, and writing—original draft; Y.A.: conceptualization, methodology, and review; and I.A.: supervision, data curation, and writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Haq, F.u., Abduljaleel, Y. & Ahmad, I. Effect of temperature on fast transmission of COVID-19 in low per capita GDP Asian countries.
Sci Rep 13, 21165 (2023). https://doi.org/10.1038/s41598-023-48587-3
-
Received: 24 March 2023
-
Accepted: 27 November 2023
-
Published: 30 November 2023
-
DOI: https://doi.org/10.1038/s41598-023-48587-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.