Research studies have shown that leveraging artificial intelligence algorithms to analyze mammogram images can help determine a person’s risk for breast cancer.


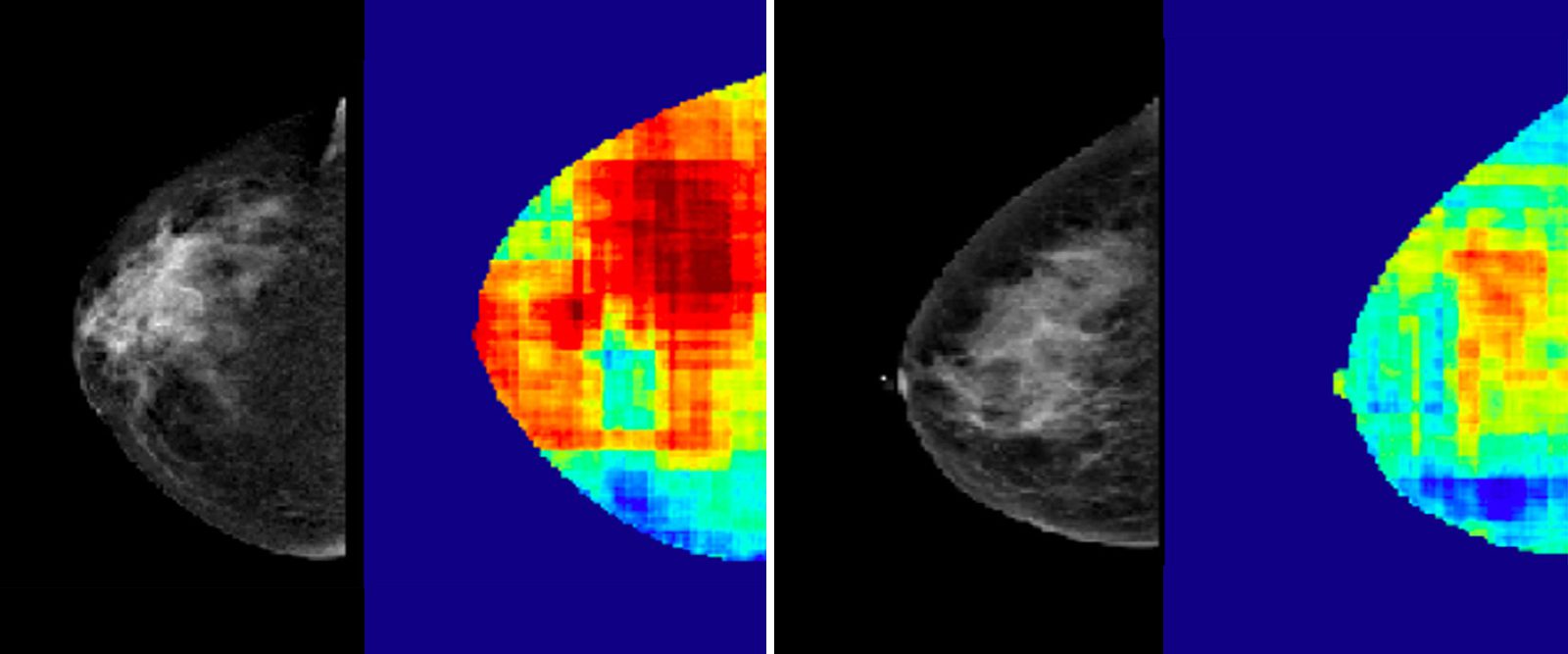
Using mammogram images of two patients who have similar breast densities, an artificial intelligence algorithm detected regions that represent high cancer risk (in red).
Breast cancer is the most common form of cancer in the world. In the United States, women have a one in eight chance of being diagnosed with breast cancer in their lifetime, according to the American Cancer Society. It is also the second-leading cause of cancer death in women.
Over the years, experts have developed various tools and technology that support screening, detection, and treatments to improve outcomes for this deadly and common disease. But what if doctors had a way to accurately predict the likelihood of someone developing breast cancer? Could prediction change the landscape for breast cancer care and survival rates?
Experts believe it can, and the development of risk prediction tools is underway thanks to artificial intelligence (AI), says Dr. Richard S Ha, acting chief of the Division of Breast Imaging at NewYork-Presbyterian/Columbia University Irving Medical Center and an associate professor of radiology at Columbia University Vagelos College of Physicians and Surgeons.
Through analyzing large amounts of data in mammogram images, deep learning — a form of AI — has been found to more accurately predict the risk of breast cancer occurrence, says Dr. Katia Dodelzon, associate attending radiologist at NewYork-Presbyterian/Weill Cornell Medical Center, vice chair of Clinical Operations for the Department of Radiology, and an associate professor of clinical radiology at Weill Cornell Medicine.
Understanding AI
According to the National Cancer Institute, implementing AI in cancer care could improve the accuracy and speed of diagnosis, aid in clinical decision-making, and lead to better health outcomes. The institute defines AI, its types, and subtypes, including deep learning, as:
- AI: “a computer performing tasks commonly associated with human intelligence. Humans code or program a computer to act, reason, and learn. An algorithm or model is the code that tells the computer how to act, reason, and learn.”
- Machine learning: “a type of AI that can learn to make predictions or decisions. The more data a machine learning model is exposed to, the better it performs over time.”
- Deep learning: “a subset of machine learning that uses artificial neural networks. A well-designed and well-trained deep learning model can perform classification tasks and make predictions with high accuracy.”
Health Matters spoke with Dr. Ha and Dr. Dodelzon to understand how these AI models work, the difference they can make in breast cancer prevention and screening, and the future of utilizing AI in breast cancer care.
How do mammogram images help AI models predict breast cancer?
Dr. Dodelzon: Mammograms are widely accessible, and they contain a wealth of information — they are immense reservoirs of data. The images allow breast radiologists to detect breast cancer and assess breast density, for example, but there is much more information contained within them. While lot of that information is not perceptible to the human eye, it is perceptible to a computer model including deep-learning models.
Dr. Ha: Mammograms contain pixels, which are tiny dots of varying brightness. Each pixel, and the way that it is connected to another pixel, can signify a relationship or pattern that may be clinically relevant. There are tens of thousands of them in an image, and the algorithm can quickly detect and analyze their patterns for potential significance.


Dr. Richard S Ha
Why are risk-prediction tools powered by AI important when it comes to a disease like breast cancer?
Dr. Ha: We need a better way to predict who is at risk because about 75% of cases occur in women who have no identifiable risk factors for breast cancer other than gender (female) and age (over 40 years) and no known genetic predisposition.
Currently, we have risk-prediction questionnaires that we use in clinical settings, such as the Tyrer-Cuzick, Gail, and Breast Cancer Surveillance Consortium models, but they can significantly underestimate risk in some women. They are questionnaires that calculate a woman’s risk score based on answers, including on their family history of the disease, breast density, and hormone replacement therapy use — a few known risk factors for breast cancer.
The most well-known imaging biomarker of breast cancer risk is breast density, with increasing density correlating with elevated risk. However, almost half (47%) of the patients in the U.S. have dense breasts in the U.S., so it may not be as useful on an individual basis.
It is important to have accurate risk-prediction tools because it can help guide screening and prevention strategies that can ultimately improve the outcome of patients.


Dr. Katia Dodelzon
How do deep learning models utilize mammogram images to make risk predictions?
Dr. Dodelzon: Once we input mammograms into the model, it analyzes the the data — the variations in pixels — and provides a score for future risk of breast cancer, based on the data and textural features that it sees in the images. We then provide the model feedback, such as ‘You were correct. This woman did develop breast cancer,’ thus further validating the risk score that it generated. We train the algorithm with mammograms of women whose outcomes we know (whether they ended up developing breast cancer or not). This allows us to continually strengthen and improve the accuracy of the algorithm.
Dr. Ha: In 2018, using a deep learning neural network, we were able to identify textural patterns within the dense regions on mammograms that were predictive of risk. Most recently, in a study published in Breast Cancer Research and Treatment in May 2023, in collaboration with our colleagues in medical oncology and in Columbia University’s Mailman School of Public Health, we showed that using our deep learning algorithm in combination with the clinical risk factors achieved the highest prediction result, particularly in African American women. This study further supports the great potential of this technology.
Subsequent studies have also found that the deep learning approach to mammogram analysis was better at predicting risk compared to breast density alone and the Tyrer-Cuzick clinical risk model.
What is the difference between utilizing AI for breast cancer risk prediction and detection?
Dr. Ha: The big difference is that for detection, the AI tool has been trained to identify regions in a mammogram that are abnormal, likely containing cancer. These are areas that can also be seen by the radiologists in most cases. For risk prediction, artificial intelligence models evaluate the mammograms of patients who do not have cancer and analyze negative mammograms for patterns that can be predictive of developing cancer many years later. This is something that cannot be seen by the radiologist.
Dr. Dodelzon: The power of AI is largely in “seeing” things that we humans cannot, such as its ability to extract and analyze additional image-based information to aid in the prognosis and prediction of breast cancer, like an individual patient’s risk assessment for future development of breast cancer or predicting response to breast cancer treatment. Its power is in doing what humans cannot, taking non-invasive evaluation, such as breast imaging, a step further to inform patient-centered and personalized screening and treatment approaches more precisely. It is a tool that arms us with the ability to do more for our patients.
AI is being studied for actual breast cancer diagnosis, but these studies are limited and outcomes variable at the moment, as there are limitations to the inherent image quality and technique, and cancer detection is a complex task. Overall, the best performances are seen when combining a breast imaging radiologist, a physician, with artificial intelligence. With further studies and improvements, the potential of this is in places where there are fewer expert breast imagers to augment their interpretative skills to a larger patient population and decrease disparities in access.
What impact can the deep learning risk-prediction model make?
Dr. Dodelzon: Ultimately, deep learning risk prediction tools can help people who are disproportionately impacted by breast cancer. Incidence and death rates differ substantially by race and ethnicity: breast cancer occurs more often among white women, but more Black women die from the disease — surpassing deaths from breast cancer in white women by 40%.
When the model is further validated, this risk assessment has the potential to be implemented in clinical settings and applied individually to each patient’s mammogram, thus providing individual breast cancer risk prediction scores which can inform and tailor individual screening strategies, identifying more accurately high-risk women who may benefit from earlier and more frequent screening.
What are the next steps?
Dr. Ha: Conducting more research studies to validate the model. It is important that the algorithm is generalizable — that it could be used widely in different populations, not only in New York but in other states and beyond. We are in the process of conducting multi-institution studies with representative demographics. Ultimately, a prospective study would be required to further validate this approach before it can be widely adopted for clinical use.
Dr. Dodelzon: At NewYork-Presbyterian/Columbia University Irving Medical Center and NewYork-Presbyterian/Weill Cornell Medical Center, we are in the process of exposing the deep learning model to a greater diversity of patient populations. We are working on expanding this study to continue to validate, build, and perfect the model. Because it is a deep learning algorithm, it is always learning and can continually improve. The more feedback we give it, the better it is going to perform.
Richard Ha, M.D., is acting chief of the Division of Breast Imaging at NewYork-Presbyterian/Columbia University Irving Medical Center and serves as an associate professor of radiology at Columbia University Vagelos College of Physicians and Surgeons. His area of active breast cancer research is in the clinical application of AI, breast MRI, and new innovative techniques.
Katia Dodelzon, M.D., is a board-certified radiologist specializing in breast imaging and an assistant attending radiologist at NewYork-Presbyterian/Weill Cornell Medical Center. She is vice chair of Clinical Operations for the Department of Radiology, an associate professor of clinical radiology, and associate program director of the Breast Imaging Fellowship Training Program at Weill Cornell Medicine.
Share This Story