Abstract
The recruitment maneuver (RM) combined with PEEP to prevent atelectasis have beneficial effects. However, the change in tidal volume (VT) due to RM combined with PEEP in pediatric patients during the induction of general anesthesia is unknown. Therefore, we assessed the effects of RM combined with PEEP on VT. Pediatric patients were divided into three groups: infants, preschool children, and school children. The RM was performed by maintaining pressure control continuous mandatory ventilation (PC-CMV) with a 15 cmH2O and PEEP increase of 5 cmH2O. VT, respiratory function and hemodynamics were monitored before and after RM combined with PEEP. VT (mL) /ideal body weight (kg) before vs. after RM combined with PEEP were 9 vs 12 mL/kg (p < 0.05) in the infants, 9 vs 11 mL/kg (p < 0.05) in the preschool children, 8 vs 10 mL/kg (p < 0.05) in the school children, respectively. HR and BP before and after RM combined with PEEP increased by 2–3% and decreased by 4–7% in all groups. RM combined with PEEP resulted in an increase in VT per ideal body weight (1.1–1.2%). Therefore, this RM combined with PEEP method might improve the lung function in pediatric patients.
Introduction
General anesthesia with tracheal intubation and mechanical ventilation is widely used in patients undergoing a variety of surgical procedures1,2,3. However, alveolar collapse is multifactorial in origin and begins quickly after tracheal intubation4,5. Reduced lung compliance6,7,8 and pulmonary gas exchange impairment may result in decreased oxygenation of arterial blood9,10,11. Absorption atelectasis occurs when the flux of oxygen from the alveoli into the capillaries exceeds that of the waste gas returning to the alveoli5,12,13. The atelectasis might increase the risk of volutrauma as a constant volume is imparted to a dwindling alveolar volume1,6. This frequently occurs during induction of general anesthesia when the fraction of inspired oxygen (FiO2) is increased to 100% and it is demonstrated on lung ultrasound and computed tomography (CT) scans of the chest1,8,9,14,15,16. Younger children and infants are especially vulnerable to hypoxemia due to their smaller functional residual capacity (FRC)4,8,12,13. Desaturation can subsequently occur by intubation or mask ventilation. Manual ventilation with increased FiO2 and the fresh gas flow is then required to recover oxygen saturation (SpO2) levels.
Various ventilatory strategies have been proposed to improve gas exchange during general anesthesia1,6,7,14,15,16. Positive end-expiratory pressure (PEEP) is demonstrated as sufficient to minimize atelectasis. It induces only a modest increase in partial pressure of oxygen (PaO2)1,17,18,19.
Recruitment maneuver (RM) are ventilation strategies aiming to re-expand atelectatic lung and improve lung compliance1,9,12. Recently, a strategy of reopening the atelectatic lung areas during anesthesia with a RM combined with PEEP has been recommended1,4,5,6. It has been shown to improve oxygenation and restore lung volume and may reduce the heterogeneity of VT distribution1,4,5,6,20,21,22.
However, the change in VT due to RM combined with PEEP after induction of general anesthesia remains unknown. Therefore, we assessed the effects of RM and PEEP on VT and hemodynamics and respiratory function in pediatric patients.
Methods
Study design
This prospective observational study was approved by the Ethics Review Board of Kyushu University Hospital (Approval No. 30-446) and was registered with the UMIN Clinical Trials Registry (no. 000050120). The study was conducted from January 2019 to May 2022. The subjects included patients who underwent dental treatment and oral maxillofacial surgery at Kyushu University Hospital under general anesthesia. Patients with upper respiratory tract or preoperative lung disease were excluded from the study. Written informed consent was obtained from the legal guardians of the eligible children before general anesthesia. Pediatric patients (American Society of Anesthesiologists-physical status (ASA-PS): 1–2; aged 3 months–10 years) who underwent general anesthesia for elective dental treatment or oral surgery were divided into three groups: infants ( years).
Anesthesia
Patients were transferred to the operating room without premedication. Anesthesia was then induced by the inhalation of 1–8% sevoflurane after beginning non-invasive monitoring of SpO2 by pulse oximetry, electrocardiography (ECG), and non-invasive blood pressure (BP) and heart rate (HR) checks. After loss of consciousness, the sevoflurane concentration was adjusted according to each patient’s hemodynamic condition.
In cases of airway obstruction, airway and jaw thrusts were applied to relieve the obstruction, and ventilation was gently assisted, as necessary. Atropine, fentanyl, and remifentanil were administered after peripheral intravenous access was achieved. Intubation was facilitated with rocuronium, using a Macintosh laryngoscope (Smiths Medical Japan, Tokyo, Japan). The size of the endotracheal tube (ETT) was judged to be appropriate when air leakage was observed at an airway pressure of 10–30 cmH2O. When air leakage was either not observed at 30 cmH2O or observed below 10 cmH2O, the ETT was replaced by another one size above or below23,24. The choice of anesthetic maintenance was determined by each anesthesiologist. Pressure control continuous mandatory ventilation (PC-CMV) was performed using a Datex-Ohmeda Aestiva (GE Healthcare, Madison, WI, USA). Anesthesia was maintained using inhalational anesthetics such as sevoflurane, isoflurane, and desflurane, with the administration of fentanyl and remifentanil for analgesia to all patients.
Following tracheal intubation, PC-CMV was initiated with 15 cmH2O and a PEEP of 4 cmH2O, inspiratory: expiratory ratio of 1:2, and initial ventilatory rate with end-tidal carbon dioxide maintained at 35–45 mmHg by adjusting the respiratory rate (15–20 breaths/min). The FiO2 was set to 1.0 throughout the study period and 0.4 during procedures.
Study intervention
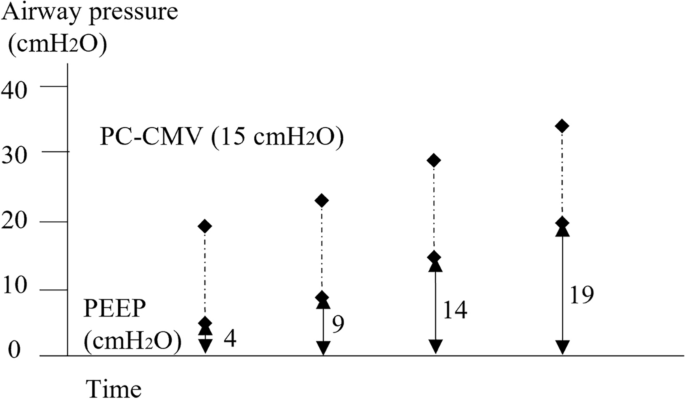
The RM was manually performed by PC-CMV with a fixed 15 cmH2O driving pressure for 5 s and a step-by-step PEEP increase of 5 cmH2O for 3 respiratory cycles up to the target level of 34 cmH2O (Fig. 1), followed by maintenance with the previous ventilator settings. This study protocol was stopped immediately if HR and/or SpO2 changed by at least 15% from baseline values.

Study protocol. Mechanics of performing the recruitment maneuver (RM) combined with positive end-expiratory pressure (PEEP). The RM was manually performed by pressure control continuous mandatory ventilation with a fixed 15 cmH2O driving pressure for 5 s and a step-by-step PEEP increase of 5 cmH2O for 3 respiratory cycles up to the target level of 34 cmH2O.
VT at end-expiration at the anesthesia ventilatory monitor, HR, BP and SpO2 for 2 min were recorded by an independent observer before and after RM combined with PEEP. The positions of the patients remained unchanged during the measurement period. Following the study protocol, procedure was performed as planned.
Data analysis
There were no previous studies can be used as a reference. An a priori power analysis was performed using 10 data points based on our clinical experiences. The sample size of 18 patients was calculated based on α = 0.05, standard deviation (SD), and a power of 80% using JMP® 15 (SAS Institute Inc., Cary, NC, USA). Factoring in an estimated dropout rate of approximately 10%, the total sample size for this study was set to 60 patients. The paired t-test was used to compare groups for nonparametric data using MATLAB (version 2015a; MathWorks, Inc., Natick, MA, USA). All values are expressed as the mean ± SD or number (n). The significance level was set at p < 0.05.
Ethics approval and consent to participate
This prospective observational study protocol was approved by Ethics Review Board of Kyushu University Hospital (Approval No.30-446). Confirming informed consent was obtained from all study participants. Moreover, all methods were carried out in accordance with relevant guidelines and regulations.
Results
In total, 60 patients were included, with 20 in each group (Table 1). No patients required swapping the ETT. VT at end-expiration before and after RM combined with PEEP were 61.8 ± 9.7 and 80.1 ± 13.9 mL (p < 0.05) in the infant group, 135.8 ± 28.5 and 164.0 ± 36.9 mL (p < 0.05) in the preschool children group, and 217.7 ± 49.7 and 246.9 ± 50.1 mL (p < 0.05) in the school children group, respectively (Table 2). In VT per ideal body weight, similar results were obtained, there were significant differences were observed between before and after RM combined with PEEP in all groups (p < 0.05) (Table 2).
The HR increased by 2–3% and the BP decreased by 4–7% after RM combined with PEEP in all groups. RM combined with PEEP resulted in an increase in VT per ideal body weight (1.1–1.2%) without respiratory (desaturation, barotrauma) or hemodynamic (hypotension) complications.
Discussion
In this prospective observational study, we compared VT at end-expiration before and after RM combined with PEEP in mechanically ventilated pediatric patients after the induction of anesthesia. VT after RM combined with PEEP significantly increased (12–18%; 19–29 mL) using PC-CMV with a high driving pressure (15 cmH2O) in normal lung, and the VT per ideal body weight was the almost same among the three groups. Furthermore, no hemodynamic or respiratory complications were observed.
Children, most particularly infants, are at an increased risk of developing atelectasis, because of the proximity of the residual volume to the closing volume of the lung and the absence of pathways for collateral ventilation12,13,21,22. They have a relatively lower FRC because the highly compliant nature of their chest wall has a reduced ability to counteract the inward elastic recoil of the lung tissue4,7. In clinical practice, 100% oxygen has been used as a standard during induction of general anesthesia including tracheal intubation, because it provides the patient enough time to tolerate apnea, it may promote atelectasis formation frequently and immediately (within a few minutes)5,6,7,13. Then, early and active management after induction of anesthesia is need by RM combined with PEEP1,5,6,8.
PEEP might be associated with alveolar collapse related to local compression atelectasis caused by overdistended upper lobes1,6,12. However, PEEP alone is insufficient in improving oxygenation5,7,13. Indeed, PEEP might increase the normally aerated lung fraction along with a reduction in the proportion of poorly aerated lung tissue, although the extent of atelectasis may remain unchanged5,8. It is important to maintain PEEP above alveolar closing pressures to prevent de-recruitment following re-expansion of atelectatic lung4,5. In contrast, it was reported that PEEP might increase intracranial pressure (IOP), and central venous pressure9,20,25,26,27.
The RM might be an important component of a lung-protective ventilation strategy to re-expand the atelectatic lungs and improve lung compliance4,7. High inspiratory pressures (around 40 cmH2O) are required to re-open collapsed alveoli, and these must be maintained for a sufficient period of time to allow lung units with slow time constants to re-expand15,28.
It was reported that RM combined other levels of PEEP was caused a significant increase in FRC, and effect on the oxygenation for a few hours and lung mechanics in concert with a significant decrease in dead space fraction, although no consensus has been reached on the ideal recruitment strategy1,18,19,22,28. This may reduce the amount of pulmonary shunt, despite a concomitant increase in perfusion to poorly ventilated lung units (low VA/Q), which might result in a small but significant reduction in PAO2-PaO21,4,5,6,18.
To the best of our knowledge, no study has assessed the effects of VT after RM combined with PEEP. The method of using RM with a stepwise increase in PEEP (4–19 cmH2O) sustained inflation of the lungs to a specific peak inspiratory pressure of 34 cmH2O based on previous reports1,6,9,14,20,21.
We suggest that an increase in VT of about a few ml per body weight was effective in terms of lung compliance and atelectasis. It is also expected to lead to improved respiratory system elastance and dead space, although we did not directly assess on CT or PaO2. Pulmonary vascular resistance is greatly increased, or decreased venous return, cardiac output (CO), and HR might occur when ventilating below or above FRC25. However, such effects are expected to be transient, with BP and CO returning to the baseline within several minutes, and serious complications may not be common.
Our study had several limitations. First, the use of FiO2 1.0 may have contributed to an increase in the amount of reabsorption atelectasis. However, the use of high FiO2 in pediatric anesthetic practice is common; pediatric patients can desaturate rapidly, and respiratory adverse events associated with airway obstruction are frequent, then it was maintained until the beginning of procedures. Second, our patients were graded ASA PS 1–2. The use of RM combined with PEEP in more unstable patients such as acute lung injury was not tested and could increase the side effects.
Conclusion
The RM combined with a stepwise increase in PEEP significantly increased VT by 12–18% (19–29 mL) without respiratory or hemodynamic complications after the induction of anesthesia. Therefore, this method may safely improve the lung function in pediatric patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
-
Hartland, B. L., Newell, T. J. & Damico, N. Alveolar recruitment maneuvers under general anesthesia: A systematic review of the literature. Respir. Care 60(4), 609–620 (2015).
Google Scholar
-
Gao, Q., Ji, H. & Wu, Z. Zhao P Effect of ultrasound-guided lung recruitment manoeuvre on perioperative atelectasis during laparoscopy in young infants: A randomised controlled trial. J. Clin. Anesth. 86, 111075 (2023).
Google Scholar
-
Tsukamoto, M., Taura, S., Hitosugi, T., Kawakubo, Y. & Yokoyama, T. Age-related effects of three inhalational anesthetics at 1 minimum alveolar concentration on electroencephalogram waveform. Aging Clin. Exp. Res. 32(9), 1857–1864 (2020).
Google Scholar
-
Bruins, S., Sommerfield, D., Powers, N. & von Ungern-Sternberg, B. S. Atelectasis and lung recruitment in pediatric anesthesia: An educational review. Paediatr. Anaesth. 32(2), 321–329 (2022).
Google Scholar
-
Bruins, S., Powers, N., Sommerfield, D. & von Ungern-Sternberg, B. S. Impact of airway and a standardized recruitment maneuver on CT chest imaging quality in a pediatric population: A retrospective review. Paediatr. Anaesth. 32(4), 572–576 (2022).
Google Scholar
-
Rothen, H. U. et al. Dynamics of re-expansion of atelectasis during general anaesthesia. Br. J. Anaesth. 82(4), 551–556 (1999).
Google Scholar
-
Whalen, F. X. et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth. Analg 102(1), 298–305 (2006).
Google Scholar
-
Futier, E. et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology 113(6), 1310–1319 (2010).
Google Scholar
-
Wu, L. et al. Modified lung ultrasound examinations in assessment and monitoring of positive end-expiratory pressure-induced lung reaeration in young children with congenital heart disease under general anesthesia. Pediatr. Crit. Care Med. 20(5), 442–449 (2019).
Google Scholar
-
Wagner, P. D. The physiological basis of pulmonary gas exchange: Implications for clinical interpretation of arterial blood gases. Eur. Respir. J. 45(1), 227–243 (2015).
Google Scholar
-
Kjaergaard, S. et al. Hypoxaemia after cardiac surgery: Clinical application of a model of pulmonary gas exchange. Eur. J. Anaesthesiol. 21(4), 296–301 (2004).
Google Scholar
-
Lebossé, M. et al. Ventilation in pediatric anesthesia: A French multicenter prospective observational study (PEDIAVENT. Paediatr. Anaesth. 30(8), 912–921 (2020).
Google Scholar
-
Song, I. K. et al. Effects of an alveolar recruitment manoeuvre guided by lung ultrasound on anaesthesia-induced atelectasis in infants: A randomised, controlled trial. Anaesthesia 72(2), 214–222 (2017).
Google Scholar
-
Boriosi, J. P. et al. Efficacy and safety of lung recruitment in pediatric patients with acute lung injury. Pediatr. Crit. Care Med. 12(4), 431–436 (2011).
Google Scholar
-
Hedenstierna, G. & Rothen, H. U. Atelectasis formation during anesthesia: Causes and measures to prevent it. J. Clin. Monit. Comput. 16(5–6), 329–335 (2000).
Google Scholar
-
Serafini, G. et al. Pulmonary atelectasis during paediatric anaesthesia: CT scan evaluation and effect of positive endexpiratory pressure (PEEP). Paediatr. Anaesth. 9(3), 225–228 (1999).
Google Scholar
-
Ahn, S., Byun, S. H., Chang, H., Koo, Y. B. & Kim, J. C. Effect of recruitment maneuver on arterial oxygenation in patients undergoing robot-assisted laparoscopic prostatectomy with intraoperative 15 cmH2O positive end expiratory pressure. Korean J. Anesthesiol. 69(6), 592–598 (2016).
Google Scholar
-
Cui, Y. et al. The effect of lung recruitment maneuvers on post-operative pulmonary complications for patients undergoing general anesthesia: A meta-analysis. PLoS One 14(5), e0217405 (2019).
Google Scholar
-
Pereira, S. M. et al. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology 129(6), 1070–1081 (2018).
Google Scholar
-
Serita, R., Morisaki, H. & Takeda, J. An individualized recruitment maneuver for mechanically ventilated patients after cardiac surgery. J. Anesth. 23(1), 87–92 (2009).
Google Scholar
-
Tusman, G. et al. Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology. 98(1), 14–22 (2003).
Google Scholar
-
Acosta, C. M. et al. Lung recruitment prevents collapse during laparoscopy in children: A randomised controlled trial. Eur. J. Anaesthesiol. 35(8), 573–580 (2018).
Google Scholar
-
Tsukamoto, M., Taura, S., Yamanaka, H., Hitosugi, T. & Yokoyama, T. Prediction of appropriate formula for nasotracheal tube size in developmental disability children. Clin. Oral Investig. 25(4), 2077–2080 (2021).
Google Scholar
-
Tsukamoto, M., Yamanaka, H. & Yokoyama, T. Predicting the appropriate size of the uncuffed nasotracheal tube for pediatric patients: A retrospective study. Clin. Oral Investig. 23(1), 493–495 (2019).
Google Scholar
-
Imanaka, H. Where should the recruitment maneuver go?. Respir. Care 57(11), 1980–1981 (2012).
Google Scholar
-
Chen, H., Zhou, J., Lin, Y. Q., Zhou, J. X. & Yu, R. G. Intracranial pressure responsiveness to positive end-expiratory pressure in different respiratory mechanics: A preliminary experimental study in pigs. BMC Neurol. 18(1), 183 (2018).
Google Scholar
-
Pulitanò, S. et al. Effects of positive end expiratory pressure (PEEP) on intracranial and cerebral perfusion pressure in pediatric neurosurgical patients. J. Neurosurg. Anesthesiol. 25(3), 330–334 (2013).
Google Scholar
-
Maisch, S. et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth. Analg 106(1), 175–181 (2008).
Google Scholar
Author information
Authors and Affiliations
Contributions
Study conception/design: M.T., T.H., T.Y. Data acquisition: M.G., M.T. Data analysis/interpretation: K.M., M.T. Final approval of the manuscript: all authors. Accuracy and integrity of the manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Tsukamoto, M., Goto, M., Hitosugi, T. et al. Comparison of the tidal volume by the recruitment maneuver combined with positive end-expiratory pressure for mechanically ventilated children.
Sci Rep 13, 18690 (2023). https://doi.org/10.1038/s41598-023-45441-4
-
Received: 10 April 2023
-
Accepted: 19 October 2023
-
Published: 31 October 2023
-
DOI: https://doi.org/10.1038/s41598-023-45441-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.