Abstract
Long COVID represents the constellation of post-acute and long-term health effects caused by SARS-CoV-2 infection; it is a complex, multisystem disorder that can affect nearly every organ system and can be severely disabling. The cumulative global incidence of long COVID is around 400 million individuals, which is estimated to have an annual economic impact of approximately $1 trillion—equivalent to about 1% of the global economy. Several mechanistic pathways are implicated in long COVID, including viral persistence, immune dysregulation, mitochondrial dysfunction, complement dysregulation, endothelial inflammation and microbiome dysbiosis. Long COVID can have devastating impacts on individual lives and, due to its complexity and prevalence, it also has major ramifications for health systems and economies, even threatening progress toward achieving the Sustainable Development Goals. Addressing the challenge of long COVID requires an ambitious and coordinated—but so far absent—global research and policy response strategy. In this interdisciplinary review, we provide a synthesis of the state of scientific evidence on long COVID, assess the impacts of long COVID on human health, health systems, the economy and global health metrics, and provide a forward-looking research and policy roadmap.
Main
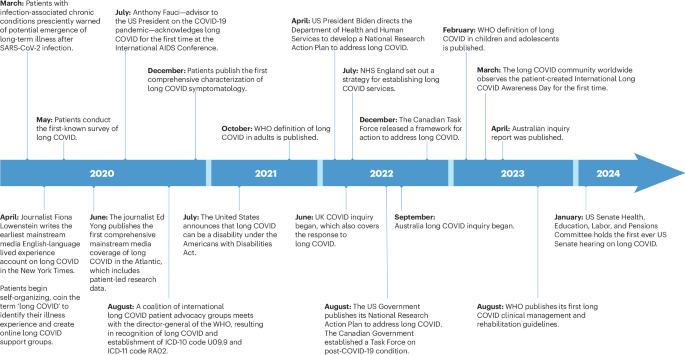
Long COVID is best defined as the constellation of post-acute and long-term health effects caused by SARS-CoV-2 infection1,2,3. Long COVID was initially reported by patients who coined the term and, through research and advocacy, drove much of the progress in understanding this condition over the past several years (Fig. 1).

The history of long COVID has been defined largely by the patients themselves. In March 2020, as the COVID-19 pandemic began to unfold across the globe, patients with infection-associated chronic conditions presciently warned of the potential emergence of long-term illness after SARS-CoV-2 infection293.The first mainstream written personal account of non-recovery from acute COVID-19 was an op-ed by the American journalist Fiona Lowenstein in the New York Times in April 2020 (ref. 294). Around the same time, patients began self-organizing, coined the term long COVID295 and conducted the first known survey—which was subsequently formally published—documenting the breadth of symptomatology experienced by people with long COVID42. Considerable activity then ensued, including mainstream media coverage (first by Ed Yong in The Atlantic)296, recognition by national governments (of the United States281, Canada297, United Kingdom298, European Union299, Australia300 and others) and the WHO. Patients continue to lead the way in advocacy and research, which led the US Senate to hold its first-ever hearing on long COVID275,301. This timeline was curated to provide a brief overview of the history of long COVID, with a focus on the role played by patients and advocates, and does not comprehensively include all events and milestones. ICD, International Classification of Diseases.
Long COVID is a complex, multisystem disorder that affects nearly every organ system, including the cardiovascular system4, the nervous system5,6,7,8, the endocrine system9,10,11, the immune system12,13, the reproductive system14 and the gastrointestinal system15. It affects people across the age spectrum (from children16,17,18 to older adults19,20), people of different race and ethnicities, sex and gender, and baseline health status21. Cardinal manifestations include brain fog (or cognitive dysfunction)7, fatigue, dysautonomia (which commonly manifests as postural orthostatic tachycardia syndrome (POTS))22 and post-exertional malaise23. Many of the health effects seen in long COVID are shared across several infection-associated chronic conditions, also called post-acute infection syndromes23,24,25,26.
The epidemiology of long COVID is influenced by various factors. The Omicron variant of SARS-CoV-2 is associated with less risk of long COVID than the Delta and pre-Delta variants27. Vaccines (before infection) and antivirals (during the acute phase of infection) may reduce the risk of long COVID. Reinfection, on the other hand, is a risk factor for long COVID28,29; even if individuals did not experience long COVID after a first SARS-CoV-2 infection, they remain at risk of developing it with subsequent infections28,29,30. Reinfection can trigger de novo long COVID or exacerbate the severity of existing long COVID28,29. Cumulatively, two infections yield a higher risk of long COVID than one infection and three infections yield a higher risk than two infections28,29.
A unifying thread of evidence across most studies evaluating the risk of long COVID is the finding that the risk increases as the severity of acute infection increases3. People who had severe COVID-19 that necessitated hospitalization exhibit a higher risk of long COVID than those with mild COVID-19. However, because most people around the globe had mild COVID-19, they constitute more than 90% of people with long COVID, despite their lower relative risk compared with that of people with severe COVID-19 (ref. 31).
Studies evaluating recovery from long COVID are sparse and inconsistent32; this is largely due to use of various definitions, incomplete accounting for all the manifestations of long COVID and misclassification of remission as ‘recovery’33. However, studies carefully evaluating individual manifestations show that recovery rates are generally low at 1 year34, and several studies show only 7–10% fully recovered at 2 years30,33,35,36. Furthermore, some manifestations of long COVID, including heart disease, diabetes, myalgic encephalomyelitis and dysautonomia are chronic conditions that last a lifetime31,37,38,39. Adding to this are the concerns about the possible emergence of new latent sequelae—that have not yet been characterized—years after the acute infection37,40,41.
The impact of long COVID is not limited to the health and well-being of individual patients and their communities. Owing to its prevalence and the breadth of its clinical manifestations42,43,44,45,46, it represents a major public health crisis47; it strains health systems and national economies, and threatens progress on global health, including the Sustainable Development Goals (SDGs).
In this interdisciplinary review, we provide a brief synthesis of the current state of scientific evidence on long COVID, including knowns, unknowns and the key controversies. We provide an assessment of the impacts of long COVID on human health, health systems, the economy and global health metrics and, finally, we provide a forward-looking research and policy roadmap that we hope will stimulate global discussion on how to address the challenge of long COVID.
State of the science on long COVID
The global burden
Estimating the global burden of long COVID presents substantial challenges due to the variability in study designs and populations, follow-up times, choice of control groups (for example, whether studies evaluated people with negative SARS-CoV-2 tests or no known SARS-CoV-2 infection as controls), assessment of baseline health before the infection (to ascertain emergence of a true new health condition) and definitions of what constitutes ‘long COVID’48,49. Variation in risk estimates also reflects the dynamic nature of the pandemic itself, which gave rise to many variants and subvariants, each yielding potentially different rates of long COVID; the effect of COVID-19 vaccines and use of antivirals in the acute phase, which may reduce the risk of long COVID; and the effect of SARS-CoV-2 reinfections, which contribute additional risk28,29.
Few countries established surveillance systems to estimate the burden of long COVID at the population level. Data from the US Centers for Disease Control and Prevention (CDC)’s National Health Interview Survey show that in 2022, 6.9% of US adults50 and 1.3% of children51 ever had long COVID. Data from the Medical Expenditure Panel Survey—a nationally representative survey of US adults—found that 6.9% of adults had ever had long COVID as of early 2023 (ref. 52). Estimates from the CDC’s Household Pulse Survey show that prevalence of current long COVID in US adults was around 6.7% in March 2024 (ref. 53). In the United Kingdom, point prevalence estimates from the Office of National Statistics show that 2.9% of the UK population (including children) were experiencing self-reported long COVID in March 2023 (ref. 54). Overall, estimates of the burden of long COVID in the general population converge around a point prevalence of 6% to 7% in adults and ~1% in children50,51,52,53,54.
Also important are estimates of the incidence of long COVID, which can be informed by high-quality meta-analyses of large-scale cohort studies among people infected with SARS-CoV-2. For instance, one analysis pooled results from 54 studies in 22 countries and estimated that approximately 6.2% of symptomatic COVID-19 survivors experience at least one of three common symptom clusters at 3 months after acute infection, across all ages and accounting for different severity levels of the initial infection and pre-COVID health status31. This analysis only considers three major symptom clusters in long COVID (fatigue with bodily pain/mood swings, and cognitive and respiratory symptom clusters); however, it sets a conservative benchmark to estimate the global risk of long COVID31.
We estimated the global incidence of long COVID on the basis of meta-regression studies that pool together all the available evidence31 (Fig. 2). Incorporating a number of assumptions, including the Institute for Health Metrics and Evaluation’s annual estimates of SARS-CoV-2 infections31,55,56,57,58,59, a proportion symptomatic cases among infections of 65% (ref. 31), and a reduction in the risk of long COVID for 2022 and 2023 to account for the putative lower severity of the Omicron variant and the effect of vaccination60, we estimated a cumulative global incidence of long COVID by the end of 2023 of approximately 400 million. It is crucial to emphasize that these estimates only represent cases arising from symptomatic infections and are likely to be conservative. The actual incidence of long COVID, including cases from asymptomatic infections61 or those with a broader range of symptoms, is expected to be higher. Furthermore, the estimates do not account for the added burden of long COVID due to reinfection29 and the possibility of latent risks (that is, risks that are not yet manifest and may emerge years or decades after infection)3,37,41. The emergence of new variants, changes in public health measures and changes in the effectiveness and uptake of vaccination may also substantially influence these estimates in the future.
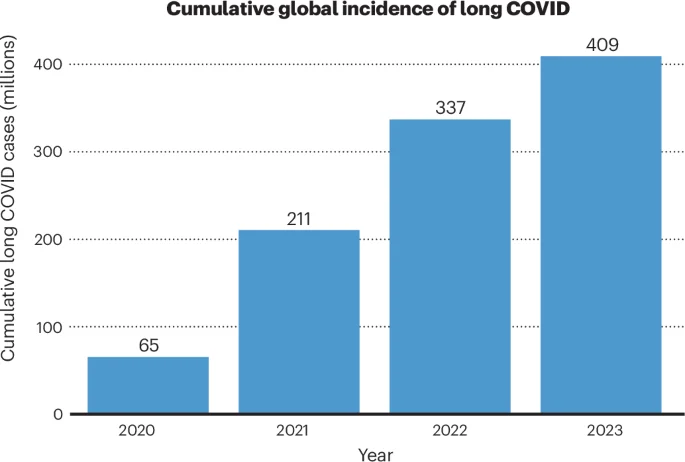
We estimated the global incidence of long COVID on the basis of meta-regression estimates that pool together all the available evidence. Considering the Institute for Health Metrics and Evaluation’s annual estimates of SARS-CoV-2 infections31,55,56,57,58,59 and assuming the lower risk estimate of 6.2% for long COVID at 3 months after infection31, a proportion symptomatic cases among infections of 65% (ref. 31), and a reduction in the risk of long COVID for 2022 and 2023 (to account for the combination of the putative lower severity of the Omicron variant and the mildly protective effect of vaccination)60, the estimated cumulative global incidence of long COVID was 65 million, 211 million, 337 million and 409 million in 2020, 2021, 2022 and 2023, respectively.
While it is challenging to provide estimates of new cases with high precision, the current evidence makes it compellingly clear that long COVID represents a substantial and ongoing challenge to global health.
Mechanisms of long COVID
The pathophysiological mechanisms of long COVID are still being elucidated2,62, and it is unlikely that a single mechanism can explain the broad and heterogeneous set of symptoms and diseases spanning various organ systems. Long COVID likely represents a disease with many subtypes; each may have their own risk factors, biological mechanisms and disease trajectory, and may respond differently to treatments3. Multiple pathological pathways may be engaged depending on various factors, including prior environmental exposures, genetic makeup, age, sex, prior health, microbiome health, viral characteristics (SARS-CoV-2 variant, viral load), the immune response (which may be influenced by prior infections, vaccines and use of immunosuppressive agents) and medical treatments (antivirals, steroids). All of these drivers likely shape the human host response during the acute phase of SARS-CoV-2 infection and may trigger pathophysiological mechanisms that ultimately produce phenotypes of long COVID.
Several mechanistic pathways have been proposed for long COVID, including viral persistence, immune dysregulation, mitochondrial dysfunction, complement dysregulation, prothrombotic inflammation and microbiome dysbiosis3,7,12,63,64,65,66,67,68,69 (Fig. 3). Viral persistence (either replicating virus or viral RNA or protein fragments)—which may be common70—in immune-privileged sites may trigger chronic low-grade inflammation and tissue injury63,71,72,73, and may correlate with long COVID symptomatology72.
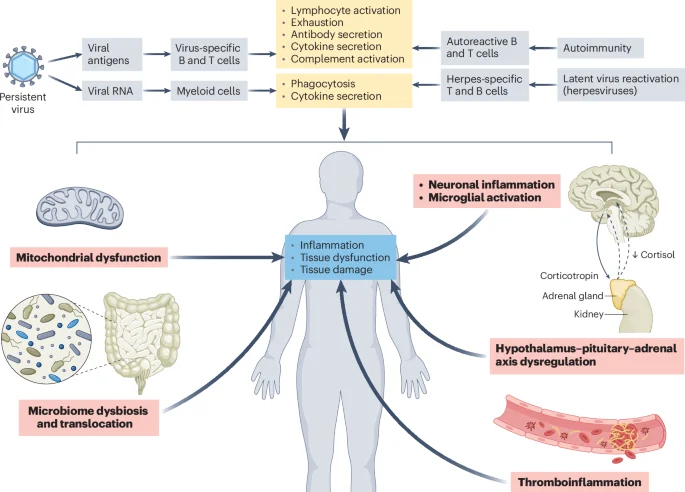
Initial triggers (gray boxes) include viral persistence in tissue reservoirs (or immune-privileged sites) and possible replication of SARS-CoV-2 leading to the generation of viral antigens and RNA, which stimulates adaptive and innate immune cells, respectively. This can lead to immune cell activation, cytokine secretion, T cell exhaustion, antibody secretion against SARS-CoV-2 antigens and complement activation (top yellow box). Innate recognition of viral RNA by myeloid cells can lead to enhanced phagocytosis and cytokine secretion and inflammasome activation (bottom yellow box). These events can trigger autoimmunity (bystander activation or molecular mimicry) and reactivation of dormant herpesviruses (EBV, VZV) and uncoordinated cross-talk between cellular and adaptive immunity. Immune activation can cause downstream pathologies (pink boxes), including mitochondrial dysfunction and impaired energy metabolism; microbiome dysbiosis and translocation and gut nervous system dysregulation; neuronal inflammation, activation of microglia and immune cells with reduced neurogenesis and loss of oligodendrocytes and myelinated axons, possible fusion between neurons and neurons and glial cells and formation of multicellular syncytia, which compromises neuronal activity; dysfunctional hypothalamic–pituitary–adrenal response leading to inappropriately low levels of cortisol; complement activation, endothelial inflammation, platelet activation and red blood cell lysis leading to thromboinflammation and tissue injury. These mechanisms are non-exclusive and may cause inflammation, tissue dysfunction and tissue damage (blue box) leading to clinical manifestations of long COVID.
Studies have demonstrated persistence of the virus in extrapulmonary sites, including the brain and coronary arteries, of individuals with severe COVID-19 (refs. 68,74). Studies in human and mouse brain organoids showed that SARS-CoV-2 infection induces fusion between neurons and between neurons and glial cells, which may progressively lead to formation of multicellular syncytia compromising neuronal activity75. Neuroimaging studies performed in humans 10 months after they ‘recovered’ from mild-to-moderate SARS-CoV-2 infection showed significant alterations (commensurate with 7 ‘years of healthy aging’) of cerebral white matter, including widespread increases of extracellular free water and mean diffusivity (indicative of inflammation) encompassing all brain lobes76. Pre- and post-SARS-CoV-2 infection imaging studies showed structural abnormalities and accelerated aging in the brains of people with mild-to-moderate SARS-CoV-2 infection74,77,78. Even in the absence of direct infection in the brain, a transient respiratory infection with SARS-CoV-2 induces prolonged neuroinflammatory responses, activation of microglial cells and impaired neurogenesis64,77. In addition to neuroinflammation, people with brain fog due to long COVID were shown to have disrupted blood–brain barriers79.
Abnormalities in the immune system have been documented in people with long COVID, including increased humoral responses directed against SARS-CoV-2; higher antibody responses against Epstein–Barr virus (EBV)66, varicella zoster virus (VZV)66 and cytomegalovirus67 (suggesting possible reactivation of herpesviruses80); exhausted T cell responses12,66; and uncoordinated cross-talk between the cellular and humoral adaptive immunity12,13. Autoimmune responses triggered by SARS-CoV-2 infection may underlie long COVID symptoms81,82. Passive transfer of IgG antibodies from patients with long COVID to healthy mice recapitulated heightened pain sensation and locomotion deficits82,83.
In the heart, SARS-CoV-2 infects coronary vessels, preferentially targeting coronary artery plaque macrophages and inducing plaque inflammation68. Vascular disease in long COVID is likely triggered by complement activation, red blood cell lysis, platelet activation and thromboinflammation—leading to altered coagulation and tissue injury67,84. Dysfunctional hypothalamic–pituitary–adrenal response with inappropriately low levels of cortisol may mediate some of the symptomatology observed in long COVID (including fatigue, sleep abnormalities and metabolic derangements)66, and has been seen in those with persistent respiratory symptoms of long COVID80. SARS-CoV-2 infection may lead to reduced intestinal absorption of tryptophan (a serotonin precursor) and subsequently reduced levels of circulating serotonin, which may impair cognition via reduced vagal signaling85. SARS-CoV-2 infection may also lead to mitochondrial dysfunction, systemic metabolic abnormalities and abnormal skeletal muscle response to exercise—including exercise-induced myopathy and tissue infiltration of amyloid-containing deposits and leukocytes65.
The proposed mechanisms of long COVID share similarities with those of other post-acute infection syndromes, which are beyond the scope of this article and are discussed in detail elsewhere24.
Prevention, treatment and care models
Non-pharmaceutical interventions (for example, masking, improved indoor air quality) can reduce the risk of SARS-CoV-2 infection and consequently reduce the risk of long COVID. COVID-19 vaccines may partially reduce the risk of long COVID in adults by 15–70% (mean, ~40%)86,87,88,89; they may also partially reduce the risk of long COVID in children90,91. In nonhospitalized individuals (mild-to-moderate COVID-19) who have at least one risk factor for the development of severe COVID-19, use of the SARS-CoV-2 antivirals (ritonavir-boosted nirmatrelvir and molnupiravir) in the acute phase may reduce the risk of long COVID92,93,94,95,96,97. However, the effectiveness of these antivirals in reducing risk of long COVID in low-risk groups, including younger individuals with no comorbidities98, has not been evaluated. Simnotrelvir—a new SARS-CoV-2 antiviral available in China99—resulted in earlier reduction in viral load and faster resolution of acute symptoms (than placebo)100, but its effectiveness against long COVID has not yet been evaluated. Exploratory analyses showed that another new SARS-CoV-2 antiviral, ensitrelvir (currently available in Japan), reduced the risk of long COVID when initiated in the acute phase of COVID-19 (refs. 101,102). Furthermore, metformin (initiated within 7 days of SARS-CoV-2 infection) has been shown to reduce the risk of long COVID in a randomized controlled trial103.
Evidence for long COVID treatments is beginning to emerge, but it is still limited. A randomized, double-blind, placebo-controlled trial showed that treatment with a synbiotic preparation (a gut microbiome modulator) alleviated multiple symptoms of long COVID—highlighting the need to further explore microbiome modulators as potential therapeutics in this setting104. Another randomized, controlled trial showed that a 15-day course of ritonavir-boosted nirmatrelvir did not reduce the burden of long COVID symptoms in comparison to ritonavir with placebo105.
Due to near-total absence of evidence from randomized clinical trials to guide treatment decisions, approaches for the assessment and treatment of respiratory sequelae106, cardiovascular complications107, fatigue108, cognitive symptoms109, autonomic dysfunction (including POTS)110,111,112,113,114 and neuropsychiatric impairment115,116 in adults and children117 are based on evidence of treating similar symptomatology from other conditions—including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Gulf War illness26,118,119,120.
Care for people with long COVID varies widely across settings and practitioners118,119,121,122,123. It is often challenged by lack of widespread recognition and understanding of long COVID among medical professionals, constrained resources and competing demands on healthcare systems still recovering from the shock of the pandemic, lack of standardized care pathways, lack of definitive diagnostic and treatment tools, and a general pervasive pandemic fatigue with an urge to ‘move on’124,125. Much of the global burden of long COVID remains undiagnosed, particularly in low-resource settings, and in many instances are erroneously attributed to psychosomatic causes126.
Overall, care models for long COVID are evolving, with substantial variability across health systems127. While there is still no empirical evidence evaluating comparative effectiveness of long COVID care models121, optimal models should be context dependent—based on available resources, expertise and the population being served121,128.
Impacts of long COVID
In addition to its impact on patients’ daily lives and health outcomes, long COVID has a devastating impact on communities and can have wide-reaching ramifications for health systems, national economies and global health metrics.
Impact on individuals and communities
Long COVID drastically affects patients’ well-being and sense of self, as well as their ability to work, socialize, care for others, manage chores and engage in community activities—which also affects patients’ families, caregivers and their communities129. Over three quarters of people with long COVID report a moderate or severe impact on general well-being130. The high rates of cognitive and physical symptoms also affect individuals’ identity and sense of self. One in four people with long COVID limit activities outside work in order to continue working131. Many patients with long COVID experience social exclusion, isolation and stigma, often from medical providers43,132,133,134. These challenges are exacerbated by societal barriers to the inclusion of people with disabilities and chronic illnesses.
Impact on health systems
Because of the large burden of long COVID and its multisystemic effects135, it has profound impacts on health systems136,137. Patients with long COVID frequently require ongoing medical care and multiple specialist consultations to manage their complex symptoms. This increased demand exacerbates existing pressures on health systems, leading to longer wait times, potential delays in essential care and increased costs. In the United States, people with long COVID are more likely to report unmet healthcare needs in the past year because of costs and difficulties finding a clinician and getting an appointment when needed138. These issues are exacerbated in low- and middle-income countries126,139. Furthermore, the lack of standardized diagnostic criteria, treatment protocols and models of care for long COVID adds to the complexity and places additional burdens on healthcare providers137,140,141.
Perhaps the most enduring challenge to health systems lies in the rise in the burden of non-communicable diseases (NCDs; for example, cardiovascular disease and diabetes) as a consequence of SARS-CoV-2 infection4,5,9,10,15,136,142,30 days after SARS-CoV-2 infection among persons aged 143,144,145,146,147,148,149,150,151,152. NCDs are chronic conditions that require lifelong care, impact health system utilization (competing for access and quality of care) and raise healthcare costs137.
Impact on economies
Long COVID strains individual financial health153 and has wide and deep ramifications on national economies154,155,156,157,158,159. In addition to the substantial direct healthcare costs160, there is also financial strain on support services and disability benefits. In addition, long COVID affects labor participation, employment and productivity of impacted individuals and their caregivers129,156,161,162,163—resulting in depleted savings, food and housing insecurity131,164 and negative impact on labor supply, thereby fueling labor shortages156. Studies indicate a significant percentage of individuals with long COVID experience a reduced ability to work or may be unable to work at all165. A report by the US Brookings Institute estimated that between 2 and 4 million US adults were out of work because of long COVID in 2022 (ref. 165). A US Federal Reserve Bank report found that people with long COVID had 10% less likelihood of being employed and worked 25% to 50% fewer hours when employed than uninfected individuals166. Survey data from the UK’s Trades Union Congress show that 20% of people with long COVID were not working and that an additional 16% were working reduced hours167. An analysis by the European Commission suggested that long COVID had a negative impact on the European labor supply of 0.2–0.3% in 2021 and 0.3–0.5% in 2022 (ref. 168).
Quantitative estimates of the total economic impact of long COVID remain preliminary. A study in 2022 estimated the economic cost of three key parameters in the United States, including lost quality of life ($2,195 billion), cost of lost earning ($997 billion) and spending on healthcare ($528 billion), for up to a total cost of $3.7 trillion154,155—this amounts to $11,000 per capita or 17% of the 2019 gross domestic product (GDP). These economic losses are on par with the global 2008 Great Recession. Assumptions included in these estimates are that burden of disability from long COVID is on par with that of ME/CFS and that long COVID lasts on average for 5 years155.
Among OECD (Organization for Economic Co-operation and Development) countries, a preliminary conservative estimate suggested that excluding the direct costs of healthcare, long COVID is likely costing OECD countries as much as $864 billion to $1.04 trillion per year due to reductions in quality of life and labor force participation169. A recent analysis by the Economist Impact (a think tank of The Economist) suggested that the economic cost of long COVID in 2024 is expected to be around 0.5% to 2.3% of the GDP of several large economies170 (Table 1). On the basis of all the available data, a conservative estimate of the annual global economic toll of long COVID could be around $1 trillion amounting to 1% of the 2024 global GDP154,155,169,170.
Impact on the SDGs
The profound immediate health, social and economic shocks triggered by the COVID-19 pandemic have undermined the ability of many countries to achieve the SDGs by 2030 (ref. 171). In addition to the immediate effect of the pandemic, its long tail—in the form of long COVID—presents a more profound and enduring challenge to SDGs than the direct initial disruptions171.
Long COVID’s multifaceted impact jeopardizes progress across many SDGs, particularly those aimed at promoting health and economic well-being, and reducing inequalities172,173,174,175,176,177,178,179. Long COVID can limit access to and quality of healthcare136,137, reduce labor participation, worsen poverty and hinder economic productivity169, and exacerbate existing inequalities180,181,182,183. Table 2 lists the impacts of long COVID on several of the SDGs and identifies which collaborative, multi-sectoral partnerships and actions are needed to address these impacts.
The full extent to which long COVID will undermine the SDGs is still evolving and is difficult to fully quantify174,175; a deeper understanding of the full scope and scale of this impact is needed.
Research and policy roadmaps
Substantial work lies ahead to address the broad and multifaceted challenges posed by long COVID—including preventing further increase in the number of people with long COVID and addressing the care needs of people already impacted184. Responding to these challenges will require coordinated, long-term policy response and visionary research strategies, guided by the principles of health equity and patient centeredness185,186,187. We developed the following research and policy roadmaps on the basis of our assessment of the evidence and policy gaps, as well as our own clinical, research and policy experience and in partnership with patients.
Research roadmap
Biological mechanisms
Leading mechanistic hypotheses (discussed above) should be examined carefully, particularly for their interactions and potential to guide disease management, trials to test existing drugs and the development of new drugs3. Continued investigation (via animal models188,189 or other approaches) of neuroinflammation, immune dysregulation, sex differences190, tissue damage and susceptibility features, including genomic191, epigenomic192,193,194 and other ‘-omics’, is warranted. In evaluating the mechanisms of long COVID, detailed assessment of specific manifestations, for example, understanding the pathophysiology of post-exertional malaise, may yield mechanistic insights that guide clinical management65,195,196.
That SARS-CoV-2 leads to long COVID is unlikely to be a unique property; many other viral agents (including influenza, SARS, Middle East respiratory syndrome, EBV, Dengue, Ebola, Polio, Chikungunya, West Nile virus, Ross River virus, Coxsackie B and VZV) and nonviral agents (Coxiella burnetii, Borrelia, Giardia lamblia) also lead to post-acute and long-term health effects24,197. A deeper understanding of the similarities and distinctions in the biological mechanisms of long COVID and other infection-associated chronic conditions is needed2,3,24,25,26,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214.
Diagnostics
A research agenda is needed to foster the development, testing and validation of more advanced imaging, new blood tests, molecular probes, ‘-omics’ and novel approaches to tissue investigation and analyses—toward better diagnosis of long COVID. Traditional imaging techniques may not reveal abnormalities in long COVID that may be evident in more advanced imaging. For example, new imaging technologies, including magnetic resonance imaging (MRI) with xenon-129 (129XE-MRI)215 for lungs, diffusion MRI to map glial activity216, imaging for glymphatic functioning217 and arterial spin labeling MRI218 for cerebral blood flow, have identified abnormalities in long COVID where conventional imaging has not. In a preliminary study, imaging flow cytometry was shown to detect fibrin microclots, which may be more abundant in people with long COVID than controls219. Whole-body positron emission tomography imaging using a highly selective radiotracer ([18F]F-AraG) that allows anatomical quantification of activated T lymphocytes, showed increased radiotracer uptake indicative of T cell activation in various anatomic sites (for example, spinal cord, lungs) that were associated with long COVID220. These imaging modalities—along with other approaches—should be further investigated for their potential to establish diagnosis of long COVID, to guide trial designs, and for targeted disease management.
Biomarkers are helpful, not only as diagnostics, but also to aid in risk stratification (to guide trials and choice of treatment), determine potential subtypes of disease, and assess severity, prognosis and response to treatment. Candidate biomarkers include immune cell phenotypes, cytokines/chemokines, immunoglobulins, complement and coagulation proteins, acute phase proteins, endocrine markers and markers of neurologic or vascular injury66,67,73,221,222. Integrated ‘-omics’ analyses223,224, including genomic, epigenomic, transcriptomic225, proteomic226,227,228, metabolomic229, lipidomic230, and microbiome231 profiling, may help identify fingerprints for various types of long COVID. However, because of the complexity of long COVID and its diverse manifestations, which likely represent distinct mechanistic pathways, a single or even a panel of laboratory tests may not achieve high-enough performance. Sequela-specific approaches for biomarker discovery may also be productive221.
In addition to imaging modalities and biomarkers, harnessing health data from wearable biosensors and other sources may also be useful for diagnosis and to identify triggers and track disease activity.
Epidemiology and clinical course
Studies to understand the incidence, prevalence, severity and trajectory of long COVID over time are critical35,36,232,233. Comprehensive understanding of risk factors, including social determinants of health, genetic, environmental, dietary, health behavior (for example, smoking) and other risks of long COVID, is also important.
Research to identify the putative subtypes (or clusters of sequelae) of long COVID has yielded variable results thus far234,235,236,237; greater clarity is needed on putative subtypes and how might they differ in terms of epidemiological features (for example, risk factors), clinical course and potential response to treatment.
Real-world evidence using high-quality data and advanced causal inference approaches (for example, target trial emulation) to evaluate effectiveness of therapeutic interventions will complement evidence generated by randomized trials238,239. This is particularly relevant in the evaluation of the long-term effects of therapeutic interventions and risks of rare adverse events; trials may have a relatively short follow-up, limiting assessment of long-term outcomes. Moreover, trials may not be adequately powered to detect rare adverse events.
Because long COVID is a new entity (it has been in existence for less than 5 years), longitudinal studies to characterize the long-term health trajectories of people with long COVID—up to 10 years, 20 years and 30 years—are needed, to understand rates and predictors of recovery and relapse of the various manifestations. These long-term studies will also help identify any latent consequences of the disease (that is, impacts that have not yet been realized) and secondary consequences (for example, the downstream health effects that emanate from long COVID). For example, understanding whether people with cognitive dysfunction (or brain fog) are at a higher risk of developing neurodegenerative diseases later in life is critical.
Comparative analyses to understand the post-acute and long-term health consequences of SARS-CoV-2 infection (and reinfection) versus other infections (for example, seasonal and pandemic influenza, respiratory syncytial virus infections and others) is important to enhance our understanding of similarities and differences in their epidemiology and clinical course197,240,241,242.
Quantifying the burden of NCDs attributable to long COVID would bring greater clarity to the extent to which billions of SARS-CoV-2 infections around the world may have impacted the global epidemiology of NCDs. The effects of long COVID on global health metrics, including SDGs, should also be periodically evaluated.
Trials to test therapeutics for long COVID
When it comes to clinical trials for long COVID therapeutics, innovation, urgency and scale are all needed243,244. Long COVID is a complex disease with many manifestations that are likely driven by several different biological mechanisms, and may need different therapeutic approaches. Approaches that reimagine trial design to incorporate the complexities of the disorder and meaningfully incorporate patient input—from trial inception to completion—are needed244,245. This may include large-scale platform trials with adaptive designs that would test a large battery of potential drug candidates to quickly identify treatments for the various forms of long COVID.
There is a large array of existing drugs that could be readily repurposed and clinically evaluated to address existing hypotheses from viral persistence to immune system dysfunction to vascular damage. Some of these drugs include SARS-CoV-2 antivirals, neutralizing monoclonal antibodies against SARS-CoV-2, non-SARS-CoV-2 antivirals (targeting reactivated EBV and VZV), immunomodulators (for example, JAK–STAT inhibitors, checkpoint inhibitors), anticoagulants, histamine 1 and 2 antagonists, metformin, GLP-1 receptor agonists, SGLT2 inhibitors, microbiome modulators, anti-inflammatory agents, and drugs that improve glymphatic functioning2,62,246. Research agendas must also include development of new antivirals and other new targeted drugs to prepare for the possibility that repurposed drugs may not be sufficiently effective247,248,249. Testing and evaluation of combinations of treatments should also be undertaken when evidence suggests complementary or synergistic mechanisms of action.
Innovation in developing and validating entry criteria and clinical endpoints for long COVID trials is also needed, along with cultivating support for these parameters from stakeholders, including regulators such as the US Food and Drug Administration and European Medicines Agency250. Endpoints must include newly developed or improved patient-reported outcomes specific to long COVID and should reflect the often cyclical or relapsing–remitting dynamic of many manifestations of long COVID—with particular focus on tracking post-exertional malaise, a pathophysiological state that impacts all collected data.
Care delivery and health systems research
Research—including comparative analyses—to evaluate the cost and effectiveness of various care pathways in improving quality of care and outcomes in people with long COVID is needed121,127,251. Research to identify and address health inequities and barriers to effective care, especially in low- and middle-income countries, in low-resource settings and in underserved communities, is essential252.
Economic impacts
The effect of long COVID on human capital253, labor participation, productivity losses (workforce absenteeism, presenteeism and disability) and other economic indicators (including job retention, career advancement and income instability) should be thoroughly evaluated. Research should explore potential disparities in the economic impact of long COVID across various demographic groups, including racial and ethnic minorities, urban and rural communities, socioeconomically marginalized populations, and individuals with preexisting health conditions.
In addition, studies are needed to quantify the direct healthcare costs associated with long COVID. The costs of disability and support systems required to address the needs of people with long COVID should be quantified. The strain that these costs pose on payors (insurance providers and governments) should also be evaluated.
Understanding the economic barriers to healthcare access and affordability for people with long COVID is also important. This includes evaluating out-of-pocket expenses, insurance coverage gaps, and disparities in access to care, rehabilitation services and support services.
Societal impacts
Long COVID affects individual lives and impacts societal well-being. Understanding the effects of long COVID on societies is important, along with understanding the social responses, the perceptions and the genesis and propagation of stigma. Improved knowledge of the social consequences of being affected by long COVID—for example, lost friendships, strained marriages and reduced ability to network—along with the interplay between them and health outcomes, will help to inform supportive interventions. It will also be important to evaluate the burden on caregivers, families and social groups.
Research to develop a deeper understanding of the causes and consequences of misinformation, disinformation and anti-science rhetoric (for example, long COVID denialism) and how to effectively combat them is also needed254. Identifying ways to improve science communication, scientific literacy and public trust in science and to bridge the science–policy gap would all help to improve public understanding, as well as the scientific and policy responses to long COVID254.
Medical anthropology should also contextualize the response of the science and medicine profession to long COVID within the broader history of medicine. This should include comparative analyses to evaluate and juxtapose the response to long COVID against the responses to the aftereffects of the 1889–1892 flu pandemic and the 1918 flu pandemic and other health crises, including the AIDS crisis in the 1980s198,199,201,255,256,257. Careful anthropologic analysis of how the medical profession approached long COVID as a new disease that emerged in the context of the COVID-19 pandemic is important. It will not only provide historic insights and greater context for our collective response, but also offer insights into how we can optimize responsiveness to emergence of new infection-associated diseases in the future.
Policy roadmap
Given the wide-ranging impact of long COVID on society and the inadequate response thus far, priorities for policy changes are vast. Policies are necessarily dependent on context, resources and various other considerations. The recommendations outlined below are general guidelines that may be adapted to fit the needs of various locales.
Prevention of long COVID
The best way to prevent long COVID is, plainly, to prevent SARS-CoV-2 infection or reinfection in the first place. Masking, especially in high-risk places258 (for example, healthcare settings), is important—along with isolation guidelines and sick leave policies that permit people with infection to recuperate at home, thereby diminishing the probability of transmission and reducing the risk of long COVID45.
Although vaccines may reduce the risk of long COVID, vaccine policies in much of the world restrict vaccine availability to high-risk groups. These policies consider risks of death and hospitalization in the acute phase (which are manifest primarily in older adults and those with comorbidities) and ignore the risk of long COVID. Adding to these policy challenges are the low rates of vaccine uptake in 2023–2024 among eligible populations259. Vaccine policies must consider the risk of long COVID, as well as the risk of hospitalization and death during the acute phase of SARS-CoV-2 infection; and strategies to improve vaccine uptake (for example, pairing the COVID-19 vaccine with the annual influenza vaccine and other approaches) should be utilized to achieve wider vaccine coverage and greater protection to populations.
Because SARS-CoV-2 is likely to remain for decades to come, it is important to develop long-term, sustainable prevention solutions. Airborne transmission risk assessment tools, such as the one developed by the World Health Organization (WHO), help inform risk reduction strategies260. Ventilation and air filtration systems can play a major role in reducing the risk of infection with airborne pathogens261. Calls have been made for mandatory improved air quality standards for public spaces and policies that would support design and equipment of homes to meet these standards261. Investment in infrastructure supporting improved indoor air quality will help reduce the risk of SARS-CoV-2 transmission and other airborne pathogens and will ensure greater resilience against future threats from airborne pathogens262. Amelioration of indoor air quality also has the added benefit of reducing risk of health effects due to indoor air pollutants263,264,265, thereby improving human health, well-being, productivity and learning261,262,266. Investment in vaccine technologies to develop more durable, variant-proof vaccines that are not rendered ineffective by ongoing mutations of the SARS-CoV-2 virus are important. Vaccine technologies that induce strong mucosal immunity to block SARS-CoV-2 infection and transmission are also needed267.
Supporting people with long COVID
Because of the considerable impacts of long COVID on people’s ability to work and care for themselves, it is imperative that an adequate response to the long COVID crisis involves ensuring people have the financial, physical and emotional support132. Streamlining of disability benefit processes, as well as increased access to home and community-based services and food and cash assistance is critical. Workplace policies that support individuals with long COVID could include flexible working hours, increased breaks to allow for pacing, the option for remote work, and sick leave policies. Funding should be provided to support patient groups and community-based organizations, which can provide and connect people to critical supports and services.
Access, quality and equity of care
Governments must work to build and expand access to long COVID care, in particular for marginalized communities (for example, rural and indigenous communities). Improving access to care may take various forms in different countries, depending on the structure of the healthcare system and the involvement of national and local governments in financially supporting healthcare services. Adequate coverage of long COVID treatments and rehabilitation services by insurance providers is requisite. Development of quality-of-care metrics for long COVID and policies to monitor and incentivize quality of care should be pursued121. As diagnostics and treatments are developed, governments must also ensure equitable access. Shining historical examples include the Brazilian National AIDS Program, which was established in 1996 in response to the HIV/AIDS crisis to ensure free and universal provision of antiretroviral drugs268,269, and the Ryan White HIV/AIDS Program (based in the United States), which provides outpatient HIV care, treatment and support services to those without health insurance and fills gaps in coverage and cost for those with insurance limitations270,271,272.
Professional education and training
Currently, very few medical schools and health professional training programs include in their curricula any meaningful training about identification and clinical management of infection-associated chronic conditions, including long COVID. A survey of physicians in the United States showed that 78% agree that long COVID is a problem but only about one-quarter feel prepared to address it273. Training of healthcare professionals to recognize and manage long COVID effectively must be prioritized. This includes embedding up-to-date information on long COVID and infection-associated chronic conditions into training curricula for health professions, as well as providing regular high-quality continuing education to qualified health providers.
Public health communication
Existing public health education on long COVID has been minimal. A survey in the United States showed that one-third of American adults still had not heard of long COVID as of August 2023 (ref. 274), and there remains very low awareness of long COVID in low- and middle-income countries. Through public education campaigns, governments must raise awareness about long COVID and the risk of chronic conditions after infection; combat social stigma across adults and children; and use a harm reduction framework to promote awareness of prevention measures (including vaccination, masking and improved indoor air quality)258,260,261.
Supporting coordinated interdisciplinary research
To achieve the research priorities listed above, governments must substantially increase the amount of funding toward research. In the United States, existing calls for the establishment of a center for infection-associated chronic conditions at the US National Institutes of Health—with a funding request of at least $1 billion per year toward long COVID research and with additional substantial funding for other infection-associated chronic conditions—should be vigorously supported275. This proposal would create a coordinating entity to lead a long-term, large-scale interdisciplinary research portfolio to address long COVID research priorities. Other governments should also explore similar proposals.
Policies supporting research should explicitly mandate meaningful patient engagement in research from inception to implementation, and should leverage existing expertise (including scientific, clinical and lived experience) in infection-associated chronic conditions. Furthermore, meaningful efforts must be made to expand the pool of researchers working on infection-associated chronic conditions, by encouraging early career scientists and clinician–researchers to focus on these conditions and providing resources to current experts to lead training and research.
Given the complexity of long COVID and its similarities to other infection-associated chronic conditions, a coordinated approach that integrates research, policy and regulatory efforts across these conditions would reduce duplication of efforts and allow a more comprehensive understanding of the common underlying mechanisms, trial designs and potential treatment strategies.
Policies from funders are needed to mandate meaningful data sharing, which will maximize the utility and pooled insights that can be generated from existing health information. Current open data protocols are insufficient, laden with bureaucratic hurdles and do not allow access to primary data, and consequently do not enable meaningful analyses. Funders must establish data banks (a pioneering exemplar of this is the UK Biobank) for the collection, storage, analysis, retrieval and dissemination of data to make long COVID research more accessible in near real time, all while upholding data privacy and data security standards276,277.
Building consensus on definitions and clinical endpoints for long COVID
Various interim definitions of long COVID exist39,278,279,280,281,282,283, but there is not yet a universal consensus on the most optimal definition—which must be sufficiently nuanced to capture the complexity of the condition and its various manifestations. It is unlikely that a single definition will fit all needs. Consensus definitions that are optimized and empirically tested for various applications, including clinical care, epidemiological surveillance, and research, should be developed. Definitions must necessarily evolve to incorporate new understanding as the evidence base for long COVID grows.
Similarly, developing consensus on clinical endpoints for trials of long COVID is needed. Drug regulatory agencies in consultation with stakeholders, including patients and scientists, should lead in this arena and provide regulatory guidance on clinical endpoints for trials. These endpoints will also have to necessarily evolve as our understanding of long COVID expands.
Building consensus on definitions and clinical endpoints would catalyze progress in this field, remove barriers to entry for the pharmaceutical industry into long COVID trials and facilitate comparative analyses across studies.
Global coordination
The global nature of long COVID necessitates international cooperation in both research and policy. International bodies (for example, the WHO) should facilitate partnership and collaboration among countries across the globe. This collaboration is pivotal to coordinate and synergize efforts across the globe and accelerate progress on the different challenges posed by long COVID.
Professional societies for long COVID
Professional societies (national and global) should be established for long COVID. Because of the multisystemic nature of long COVID (and the other infection-associated chronic conditions), it does not fit neatly under any of the traditional organ-based organizational structures of medical care and research284, hence the need for professional home(s) for long COVID and associated conditions. Dedicated professional societies could provide strategic leadership and guidance in the clinical management of long COVID and associated conditions284. They could serve as hubs to coordinate education, research and advocacy efforts284. These professional societies could play a major role in organizing and hosting national and international conferences, spearheading efforts to provide periodic synthesis of evidence that distills existing research into actionable insights guiding care of people with long COVID. The newly established Clinical Post COVID Society in the United Kingdom may be a promising example of this284.
Preparedness for the next pandemic
We must reflect on our collective experience with COVID-19 to enhance resilience and preparedness for future pandemics285,286,287. A major lesson learned from long COVID is that pandemics leave in their wake a long tail of disease and disability198. This is not unique to the COVID-19 pandemic198; historical accounts show similar phenomena following previous pandemics198,199,255. Due to climate change, deforestation, human encroachment on animal habitat, increased frequency of travel, a growing livestock industry and other anthropogenic factors, the risk of zoonotic spillover and novel viral sharing among species is likely higher in the twenty-first century than it was in the twentieth century286,288,289,290,291,292. Many of the geographic areas that are most prone to these changes are also projected to have high population density—creating ripe conditions for pandemics289,291. Future pandemics are likely to also produce long-term disability and disease198. Investment in systems to measure the population-level incidence and prevalence of post-acute and chronic disease caused by infectious agents, including SARS-CoV-2, will aid in the characterization of the epidemiology of long COVID and will position us to be better prepared to deal with post-acute and chronic illnesses that will emerge in future pandemics. Incorporating the potential emergence of long-term health effects into initiatives for pandemic preparedness and resilience (for example, the WHO Preparedness and Resilience for Emerging Threats Initiative) is essential to optimize response to the long-term consequences of future pandemics.
Conclusions
Considerable progress has been made in the past several years in characterizing the epidemiology, clinical course and biology of long COVID. But much remains to be done. The scale of long COVID and its far-reaching impacts necessitate a robust and coordinated research and policy response strategy. Addressing the research and care needs of people impacted by long COVID will have broad benefits, potentially unlocking a better understanding of infection-associated chronic illnesses (an ignored area for decades) and optimizing our preparedness for the next pandemic.
References
-
Al-Aly, Z., Xie, Y. & Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 594, 259–264 (2021).
Google Scholar
-
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21, 133–146 (2023).
Google Scholar
-
Al-Aly, Z. & Topol, E. Solving the puzzle of Long COVID. Science 383, 830–832 (2024).
Google Scholar
-
Xie, Y., Xu, E., Bowe, B. & Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 28, 583–590 (2022).
Google Scholar
-
Xu, E., Xie, Y. & Al-Aly, Z. Long-term neurologic outcomes of COVID-19. Nat. Med. 28, 2406–2415 (2022).
Google Scholar
-
Xie, Y., Xu, E. & Al-Aly, Z. Risks of mental health outcomes in people with COVID-19: cohort study. Br. Med. J. 376, e068993 (2022).
Google Scholar
-
Al-Aly, Z. & Rosen, C. J. Long COVID and impaired cognition – more evidence and more work to do. N. Engl. J. Med. 390, 858–860 (2024).
Google Scholar
-
Kim, S. et al. Short- and long-term neuropsychiatric outcomes in long COVID in South Korea and Japan. Nat. Hum. Behav. https://doi.org/10.1038/s41562-024-01895-8 (2024).
-
Xie, Y. & Al-Aly, Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol 10, 311–321 (2022).
Google Scholar
-
Xu, E., Xie, Y. & Al-Aly, Z. Risks and burdens of incident dyslipidaemia in long COVID: a cohort study. Lancet Diabetes Endocrinol. 11, 120–128 (2023).
Google Scholar
-
Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney outcomes in long COVID. J. Am. Soc. Nephrol. 32, 2851–2862 (2021).
Google Scholar
-
Yin, K. et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat. Immunol. 25, 218–225 (2024).
Google Scholar
-
Peluso, M. J., Abdel-Mohsen, M., Henrich, T. J. & Roan, N. R. Systems analysis of innate and adaptive immunity in Long COVID. Semin. Immunol. 72, 101873 (2024).
Google Scholar
-
Pollack, B. et al. Female reproductive health impacts of Long COVID and associated illnesses including ME/CFS, POTS, and connective tissue disorders: a literature review. Front. Rehabil. Sci. 4, 1122673 (2023).
Google Scholar
-
Xu, E., Xie, Y. & Al-Aly, Z. Long-term gastrointestinal outcomes of COVID-19. Nat. Commun. 14, 983 (2023).
Google Scholar
-
Zimmermann, P., Pittet, L. F. & Curtis, N. How common is Long COVID in children and adolescents? Pediatr. Infect. Dis. J. 40, e482–e487 (2021).
Google Scholar
-
Rao, S. et al. Postacute sequelae of SARS-CoV-2 in children. Pediatrics 153, e2023062570 (2024).
Google Scholar
-
Gurdasani, D. et al. Long COVID in children. Lancet Child Adolesc. Health 6, e2 (2022).
Google Scholar
-
Mansell, V., Hall Dykgraaf, S., Kidd, M. & Goodyear-Smith, F. Long COVID and older people. Lancet Healthy Longev. 3, e849–e854 (2022).
Google Scholar
-
Fung, K. W., Baye, F., Baik, S. H., Zheng, Z. & McDonald, C. J. Prevalence and characteristics of long COVID in elderly patients: An observational cohort study of over 2 million adults in the US. PLoS Med. 20, e1004194 (2023).
Google Scholar
-
Xie, Y., Bowe, B. & Al-Aly, Z. Burdens of post-acute sequelae of COVID-19 by severity of acute infection, demographics and health status. Nat. Commun. 12, 6571 (2021).
Google Scholar
-
Blitshteyn, S. & Whitelaw, S. Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: a case series of 20 patients. Immunol. Res. 69, 205–211 (2021).
Google Scholar
-
Volberding, P. A., Chu, B. X. & Spicer, C. M. Long-Term Health Effects of COVID-19 (The National Academies Press, 2024).
-
Choutka, J., Jansari, V., Hornig, M. & Iwasaki, A. Unexplained post-acute infection syndromes. Nat. Med. 28, 911–923 (2022).
Google Scholar
-
Marshall-Gradisnik, S. & Eaton-Fitch, N. Understanding myalgic encephalomyelitis. Science 377, 1150–1151 (2022).
Google Scholar
-
Komaroff, A. L. & Lipkin, W. I. ME/CFS and Long COVID share similar symptoms and biological abnormalities: road map to the literature. Front. Med. 10, 1187163 (2023).
Google Scholar
-
Xie, Y., Choi, T. & Ziyad, A.-A. Postacute sequelae of SARS-CoV-2 infection in the pre-delta, delta, and omicron eras. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2403211 (2024).
-
Kuang, S. et al. Experiences of Canadians with long-term symptoms following COVID-19. Statistics Canada https://www150.statcan.gc.ca/n1/pub/75-006-x/2023001/article/00015-eng.htm (8 December 2023).
-
Bowe, B., Xie, Y. & Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 28, 2398–2405 (2022).
Google Scholar
-
Bosworth, M. L. et al. Risk of new-onset long COVID following reinfection with severe acute respiratory syndrome coronavirus 2: a community-based cohort study. Open Forum Infect. Dis. 10, ofad493 (2023).
Google Scholar
-
Global Burden of Disease Long COVID Collaborators et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. J. Am. Med. Assoc. 328, 1604–1615 (2022).
-
Graham, F. Daily briefing: answers emerge about long COVID recovery. Nature https://doi.org/10.1038/d41586-023-02190-8 (2023).
-
Mateu, L. et al. Determinants of the onset and prognosis of the post-COVID-19 condition: a 2-year prospective observational cohort study. Lancet Reg. Health Eur. 33, 100724 (2023).
Google Scholar
-
Gutiérrez-Canales, L. G. et al. Persistence of COVID-19 symptoms and quality of life at three and twelve months after hospital discharge. Medicina 60, 944 (2024).
Google Scholar
-
Huang, L. et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet 398, 747–758 (2021).
Google Scholar
-
Zhang, H. et al. 3-year outcomes of discharged survivors of COVID-19 following the SARS-CoV-2 omicron (B.1.1.529) wave in 2022 in China: a longitudinal cohort study. Lancet Respir. Med. 12, 55–66 (2024).
Google Scholar
-
Bowe, B., Xie, Y. & Al-Aly, Z. Postacute sequelae of COVID-19 at 2 years. Nat. Med. 29, 2347–2357 (2023).
Google Scholar
-
Al-Aly, Z. Diabetes after SARS-CoV-2 infection. Lancet Diabetes Endocrinol. 11, 11–13 (2023).
Google Scholar
-
Fineberg, H. V., Brown, L., Worku, T. & Goldowitz, I. A Long COVID Definition (National Academies Press, 2024).
-
Taquet, M. et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1,284,437 patients. Lancet Psychiatry 9, 815–827 (2022).
Google Scholar
-
Cai, M., Xie, Y., Topol, E. J. & Al-Aly, Z. Three-year outcomes of post-acute sequelae of COVID-19. Nat. Med. 30, 1564–1573 (2024).
Google Scholar
-
Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 38, 101019 (2021).
Google Scholar
-
Re’em, Y. et al. Factors associated with psychiatric outcomes and coping in Long COVID. Nat. Ment. Health 1, 361–372 (2023).
Google Scholar
-
Re’em, Y., Symeonides, M. & McCorkell, L. Serology test results and other important characteristics of patients with persistent COVID-19 symptoms. JAMA Intern. Med. 182, 576–577 (2022).
Google Scholar
-
Ziauddeen, N. et al. Characteristics and impact of Long Covid: findings from an online survey. PLoS ONE 17, e0264331 (2022).
Google Scholar
-
O’Brien, K. K. et al. Conceptualising the episodic nature of disability among adults living with Long COVID: a qualitative study. BMJ Glob. Health 8, e011276 (2023).
Google Scholar
-
Blitshteyn, S. & Verduzco-Gutierrez, M. Long COVID: a major public health issue. Am. J. Phys. Med. Rehabil. https://doi.org/10.1097/PHM.0000000000002486 (2024).
-
Ledford, H. How common is long COVID? Why studies give different answers. Nature 606, 852–853 (2022).
Google Scholar
-
Woodrow, M. et al. Systematic review of the prevalence of Long COVID. Open Forum Infect. Dis. 10, ofad233 (2023).
Google Scholar
-
Adjaye-Gbewonyo, D., Vahratian, A., Perrine, C. G. & Bertolli, J. Long COVID in adults: United States, 2022. NCHS Data Brief 480, 1–8 (2023).
-
Vahratian, A., Adjaye-Gbewonyo, D., Lin, J. S. & Saydah, S. Long COVID in children: United States, 2022. NCHS Data Brief 479, 1–6 (2023).
-
Fang, Z., Ahrnsbrak, R. & Rekito, A. Evidence mounts that about 7% of US adults have had long COVID. J. Am. Med. Assoc 332, 5–6 (2024).
Google Scholar
-
National Center for Health Statistics. Long COVID: Household Pulse Survey. CDC https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm (accessed 1 July 2024).
-
UK Office of National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 30 March 2023. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/30march2023/ (30 March 2023).
-
COVID-19 Cumulative Infection Collaborators. Estimating global, regional, and national daily and cumulative infections with SARS-CoV-2 through Nov 14, 2021: a statistical analysis. Lancet 399, 2351–2380 (2022).
-
GBD 2021 Demographics Collaborators. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 403, 1989–2056 (2024).
-
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
-
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
-
GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203 (2024).
-
Antonelli, M., Pujol, J. C., Spector, T. D., Ourselin, S. & Steves, C. J. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet 399, 2263–2264 (2022).
Google Scholar
-
Ma, Y. et al. Long-term consequences of asymptomatic SARS-CoV-2 infection: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 20, 1613 (2023).
Google Scholar
-
Altmann, D. M., Whettlock, E. M., Liu, S., Arachchillage, D. J. & Boyton, R. J. The immunology of long COVID. Nat. Rev. Immunol. 23, 618–634 (2023).
Google Scholar
-
Proal, A. D. et al. SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC). Nat. Immunol. 24, 1616–1627 (2023).
Google Scholar
-
Fernández-Castañeda, A. et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell 185, 2452–2468 (2022).
Google Scholar
-
Appelman, B. et al. Muscle abnormalities worsen after post-exertional malaise in Long COVID. Nat. Commun. 15, 17 (2024).
Google Scholar
-
Klein, J. et al. Distinguishing features of long COVID identified through immune profiling. Nature 623, 139–148 (2023).
Google Scholar
-
Cervia-Hasler, C. et al. Persistent complement dysregulation with signs of thromboinflammation in active Long COVID. Science 383, eadg7942 (2024).
Google Scholar
-
Eberhardt, N. et al. SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels. Nat. Cardiovas. Res. 2, 899–916 (2023).
Google Scholar
-
Guarnieri, J. W. et al. Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts. Sci. Transl. Med. 15, eabq1533 (2023).
Google Scholar
-
Ghafari, M. et al. Prevalence of persistent SARS-CoV-2 in a large community surveillance study. Nature 626, 1094–1101 (2024).
Google Scholar
-
Peluso, M. J. et al. Plasma-based antigen persistence in the post-acute phase of COVID-19. Lancet Infect. Dis. 24, e345–e347 (2024).
Google Scholar
-
Zuo, W. et al. The persistence of SARS-CoV-2 in tissues and its association with long COVID symptoms: a cross-sectional cohort study in China. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(24)00171-3 (2024).
-
Menezes, S. M. et al. Blood transcriptomic analyses reveal persistent SARS-CoV-2 RNA and candidate biomarkers in post-COVID-19 condition. Lancet Microbe https://doi.org/10.1016/S2666-5247(24)00055-7 (2024).
-
Stein, S. R. et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature 612, 758–763 (2022).
Google Scholar
-
Martínez-Mármol, R. et al. SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity. Sci. Adv. 9, eadg2248 (2023).
Google Scholar
-
Petersen, M. et al. Brain imaging and neuropsychological assessment of individuals recovered from a mild to moderate SARS-CoV-2 infection. Proc. Natl Acad. Sci. USA 120, e2217232120 (2023).
Google Scholar
-
Monje, M. & Iwasaki, A. The neurobiology of long COVID. Neuron 110, 3484–3496 (2022).
Google Scholar
-
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022).
Google Scholar
-
Greene, C. et al. Blood-brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment. Nat. Neurosci. 27, 421–432 (2024).
Google Scholar
-
Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895 (2022).
Google Scholar
-
Chang, R. et al. Risk of autoimmune diseases in patients with COVID-19: a retrospective cohort study. EClinicalMedicine 56, 101783 (2023).
Google Scholar
-
Santos Guedes de Sa, K. et al. A causal link between autoantibodies and neurological symptoms in long COVID. Preprint at medRxiv https://doi.org/10.1101/2024.06.18.24309100 (2024).
-
Chen, H. -J. et al. Transfer of IgG from Long COVID patients induces symptomology in mice. Preprint at bioRxiv https://doi.org/10.1101/2024.05.30.596590 (2024).
-
Turner, S. et al. Long COVID: pathophysiological factors and abnormalities of coagulation. Trends Endocrinol. Metab. 34, 321–344 (2023).
Google Scholar
-
Wong, A. C. et al. Serotonin reduction in post-acute sequelae of viral infection. Cell 186, 4851–4867 (2023).
Google Scholar
-
Català, M. et al. The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia. Lancet Respir. Med. 12, 225–236 (2024).
Google Scholar
-
Trinh, N. T. et al. Effectiveness of COVID-19 vaccines to prevent long COVID: data from Norway. Lancet Respir. Med. 12, e33–e34 (2024).
Google Scholar
-
Lundberg-Morris, L. et al. COVID-19 vaccine effectiveness against post-COVID-19 condition among 589,722 individuals in Sweden: population based cohort study. Br. Med. J. 383, e076990 (2023).
Google Scholar
-
Marra, A. R. et al. The effectiveness of COVID-19 vaccine in the prevention of post-COVID conditions: a systematic literature review and meta-analysis of the latest research. Antimicrob. Steward Healthc. Epidemiol. 3, e168 (2023).
Google Scholar
-
Atchison, C. J. et al. Long-term health impacts of COVID-19 among 242,712 adults in England. Nat. Commun. 14, 6588 (2023).
Google Scholar
-
Yousaf, A. R. et al. COVID-19 mRNA vaccination reduces the occurrence of post-COVID conditions in U.S. children aged 5-17 years following omicron SARS-CoV-2 infection, July 2021-September 2022. Open Forum Infect. Dis. 10, ofad500.2466 (2023).
Google Scholar
-
Xie, Y., Bowe, B. & Al-Aly, Z. Molnupiravir and risk of hospital admission or death in adults with COVID-19: emulation of a randomized target trial using electronic health records. Br. Med. J. 380, e072705 (2023).
Google Scholar
-
Xie, Y., Bowe, B. & Al-Aly, Z. Nirmatrelvir and risk of hospital admission or death in adults with covid-19: emulation of a randomized target trial using electronic health records. Br. Med. J. 381, e073312 (2023).
Google Scholar
-
Gottlieb, R. L. et al. Early remdesivir to prevent progression to severe COVID-19 in outpatients. N. Engl. J. Med. 386, 305–315 (2022).
Google Scholar
-
Xie, Y., Choi, T. & Al-Aly, Z. Molnupiravir and risk of post-acute sequelae of COVID-19: cohort study. Br. Med. J. 381, e074572 (2023).
Google Scholar
-
Xie, Y., Choi, T. & Al-Aly, Z. Association of treatment with nirmatrelvir and the risk of post-COVID-19 condition. JAMA Intern. Med. 183, 554–564 (2023).
Google Scholar
-
Fung, K. W., Baye, F., Baik, S. H. & McDonald, C. J. Nirmatrelvir and molnupiravir and post–COVID-19 condition in older patients. JAMA Intern. Med. 183, 1404–1406 (2023).
Google Scholar
-
Hammond, J. et al. Nirmatrelvir for vaccinated or unvaccinated adult outpatients with COVID-19. N. Engl. J. Med. 390, 1186–1195 (2024).
Google Scholar
-
Jiang, X. et al. Structure-based development and preclinical evaluation of the SARS-CoV-2 3C-like protease inhibitor simnotrelvir. Nat. Commun. 14, 6463 (2023).
Google Scholar
-
Cao, B. et al. Oral simnotrelvir for adult patients with mild-to-moderate COVID-19. N. Engl. J. Med. 390, 230–241 (2024).
Google Scholar
-
Antar, A. A. R. & Peluso, M. J. CROI 2023: acute and post-acute COVID-19. Top. Antivir. Med 31, 493–509 (2023).
Google Scholar
-
Yotsuyanagi, H. et al. Prevention of post COVID-19 condition by early treatment with ensitrelvir in the phase 3 SCORPIO-SR trial. Antiviral Res. 229, 105958 (2024).
-
Bramante, C. T. et al. Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial. Lancet Infect. Dis. 23, 1119–1129 (2023).
Google Scholar
-
Lau, R. I. et al. A synbiotic preparation (SIM01) for post-acute COVID-19 syndrome in Hong Kong (RECOVERY): a randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 24, 256–265 (2024).
Google Scholar
-
Geng, L. N. et al. Nirmatrelvir-ritonavir and symptoms in adults with postacute sequelae of SARS-CoV-2 infection: the STOP-PASC randomized clinical trial. JAMA Intern. Med. 7, e242007 (2024).
-
Maley, J. H. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of breathing discomfort and respiratory sequelae in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 14, 77–95 (2022).
Google Scholar
-
Whiteson, J. H. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of cardiovascular complications in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 14, 855–878 (2022).
Google Scholar
-
Herrera, J. E. et al. Response to letter to the editor regarding ‘multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of fatigue in patients with post-acute sequelae of SARS-CoV-2 infection (PASC)’. PM R. 13, 1439–1440 (2021).
Google Scholar
-
Fine, J. S. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of cognitive symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 14, 96–111 (2022).
Google Scholar
-
Blitshteyn, S. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 14, 1270–1291 (2022).
Google Scholar
-
Raj, S. R. et al. Canadian Cardiovascular Society Position Statement on postural orthostatic tachycardia syndrome (POTS) and related disorders of chronic orthostatic intolerance. Can. J. Cardiol. 36, 357–372 (2020).
Google Scholar
-
Espinosa-Gonzalez, A. B. et al. Orthostatic tachycardia after COVID-19. Br. Med. J. 380, e073488 (2023).
Google Scholar
-
Fedorowski, A. et al. Cardiovascular autonomic dysfunction in post-COVID-19 syndrome: a major health-care burden. Nat. Rev. Cardiol. 21, 379–395 (2024).
Google Scholar
-
Fedorowski, A. & Sutton, R. Autonomic dysfunction and postural orthostatic tachycardia syndrome in post-acute COVID-19 syndrome. Nat. Rev. Cardiol. 20, 281–282 (2023).
Google Scholar
-
Cheng, A. L. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of mental health symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 15, 1588–1604 (2023).
Google Scholar
-
Melamed, E. et al. Multidisciplinary collaborative consensus guidance statement on the assessment and treatment of neurologic sequelae in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 15, 640–662 (2023).
Google Scholar
-
Malone, L. A. et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of postacute sequelae of SARS-CoV-2 infection (PASC) in children and adolescents. PM R. 14, 1241–1269 (2022).
Google Scholar
-
Greenhalgh, T. & Knight, M. Long COVID: a primer for family physicians. Am. Fam. Physician 102, 716–717 (2020).
Google Scholar
-
Greenhalgh, T., Sivan, M., Delaney, B., Evans, R. & Milne, R. Long COVID—an update for primary care. Br. Med. J. 378, e072117 (2022).
Google Scholar
-
Palacio, A., Bast, E., Klimas, N. & Tamariz, L. Lessons learned in implementing a multidisciplinary long COVID clinic. Am. J. Med. https://doi.org/10.1016/j.amjmed.2024.05.020 (2024).
-
Greenhalgh, T., Darbyshire, J. L., Lee, C., Ladds, E. & Ceolta-Smith, J. What is quality in long covid care? Lessons from a national quality improvement collaborative and multi-site ethnography. BMC Med. 22, 159 (2024).
Google Scholar
-
Sunkersing, D. et al. What is current care for people with Long COVID in England? A qualitative interview study. BMJ Open 14, e080967 (2024).
Google Scholar
-
Heightman, M. et al. Post-COVID-19 assessment in a specialist clinical service: a 12-month, single-centre, prospective study in 1325 individuals. BMJ Open Respir. Res. 8, e001041 (2021).
Google Scholar
-
Clutterbuck, D. et al. Barriers to healthcare access and experiences of stigma: Findings from a coproduced Long Covid case-finding study. Health Expect. 27, e14037 (2024).
Google Scholar
-
Routen, A. et al. Understanding and tracking the impact of long COVID in the United Kingdom. Nat. Med. 28, 11–15 (2022).
Google Scholar
-
Ledford, H. Long COVID is a double curse in low-income nations – here’s why. Nature 625, 20–22 (2024).
Google Scholar
-
Chou, R. et al. Long COVID definitions and models of care: a scoping review. Ann. Intern. Med. https://doi.org/10.7326/M24-0677 (2024).
-
Turk, F. et al. Pathways to care for Long COVID and for long-term conditions from patients’ and clinicians’ perspective. J. Evid. Based Med. 16, 435–437 (2023).
Google Scholar
-
Kwon, J. et al. Impact of Long COVID on productivity and informal caregiving. Eur. J. Health. Econ. https://doi.org/10.1007/s10198-023-01653-z (2023).
-
O’Mahony, L. et al. Impact of Long COVID on health and quality of life. HRB Open Res 5, 31 (2022).
Google Scholar
-
Karpman, M. et al. Employment and material hardship among adults with long COVID in December 2022. Urban Institute https://www.urban.org/sites/default/files/2023-07/Employment%20and%20Material%20Hardship%20among%20Adults%20with%20Long%20COVID%20in%20December%202022.pdf (July 2023).
-
McNabb, K. C. et al. ‘It was almost like it’s set up for people to fail’ A qualitative analysis of experiences and unmet supportive needs of people with Long COVID. BMC Public Health 23, 2131 (2023).
Google Scholar
-
Hossain, M. M. et al. Living with ‘long COVID’: a systematic review and meta-synthesis of qualitative evidence. PLoS ONE 18, e0281884 (2023).
Google Scholar
-
Au, L., Capotescu, C., Eyal, G. & Finestone, G. Long COVID and medical gaslighting: dismissal, delayed diagnosis, and deferred treatment. SSM Qual. Res. Health 2, 100167 (2022).
Google Scholar
-
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27, 601–615 (2021).
Google Scholar
-
Al-Aly, Z., Agarwal, A., Alwan, N. & Luyckx, V. A. Long COVID: long-term health outcomes and implications for policy and research. Nat. Rev. Nephrol. 19, 1–2 (2023).
Google Scholar
-
Katz, G. M. et al. Understanding how post–COVID-19 condition affects adults and health care systems. JAMA Health Forum 4, e231933 (2023).
Google Scholar
-
Karpman, M., Zuckerman, S. & Morriss, S. Health care access and affordability among US adults aged 18 to 64 years with self-reported post-COVID-19 condition. JAMA Netw. Open 6, e237455 (2023).
Google Scholar
-
Jassat, W. et al. Long COVID in low-income and middle-income countries: the hidden public health crisis. Lancet 402, 1115–1117 (2023).
Google Scholar
-
Menges, D. et al. Burden of post-COVID-19 syndrome and implications for healthcare service planning: a population-based cohort study. PLoS ONE 16, e0254523 (2021).
Google Scholar
-
Greenhalgh, T., Knight, M., A’Court, C., Buxton, M. & Husain, L. Management of post-acute COVID-19 in primary care. Br. Med. J. 370, m3026 (2020).
-
Bull-Otterson, L. et al. Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 years—United States, March 2020–November 2021. MMWR Morb. Mortal. Wkly Rep. 71, 713–717 (2022).
Google Scholar
-
Barrett, C. E. et al. Risk for newly diagnosed diabetes >30 days after SARS-CoV-2 infection among persons aged <18 years—United States, March 2020–June 2021. MMWR Morb. Mortal. Wkly Rep. 71, 59–65 (2022).
-
Zhang, T. et al. Risk for newly diagnosed diabetes after COVID-19: a systematic review and meta-analysis. BMC Med. 20, 444 (2022).
Google Scholar
-
Koyama, A. K. et al. Risk of cardiovascular disease after COVID-19 diagnosis among adults with and without diabetes. J. Am. Heart Assoc. 12, e029696 (2023).
Google Scholar
-
Wang, W., Wang, C. -Y., Wang, S. -I. & Wei, J. C. -C. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: a retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine 53, 101619 (2022).
Google Scholar
-
Ayoubkhani, D. et al. Post-Covid syndrome in individuals admitted to hospital with COVID-19: retrospective cohort study. Br. Med. J. 372, n693 (2021).
Google Scholar
-
Lawson, C. A. et al. Long COVID and cardiovascular disease: a prospective cohort study. Open Heart 11, e002662 (2024).
Google Scholar
-
Roca-Fernandez, A. et al. Cardiac abnormalities in Long COVID 1-year post-SARS-CoV-2 infection. Open Heart 10, e002241 (2023).
Google Scholar
-
Dennis, A. et al. Multi-organ impairment and long COVID: a 1-year prospective, longitudinal cohort study. J. R. Soc. Med 116, 97–112 (2023).
Google Scholar
-
O’Mahoney, L. L. et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine 55, 101762 (2023).
-
Al-Aly, Z. & Cao, B. The enduring effect of the COVID-19 pandemic on diabetes. Lancet Diabetes Endocrinol. 12, 508–510 (2024).
Google Scholar
-
Rhead, R. et al. Long COVID and financial outcomes: evidence from four longitudinal population surveys. J. Epidemiol. Community Health 78, 458–465 (2024).
Google Scholar
-
Cutler, D. M. The costs of long COVID. JAMA Health Forum 3, e221809 (2022).
Google Scholar
-
Cutler, D. The economic cost of long COVID: an update. Harvard Kennedy School https://scholar.harvard.edu/sites/scholar.harvard.edu/files/cutler/files/long_covid_update_7-22.pdf (2022).
-
Reuschke, D. & Houston, D. The impact of Long COVID on the UK workforce. Appl. Econ. Lett. 30, 2510–2514 (2023).
Google Scholar
-
Gandjour, A. Long COVID: costs for the German economy and health care and pension system. BMC Health Serv. Res. 23, 641 (2023).
Google Scholar
-
Alexandri, E. et al. The economic burden of Long Covid in the UK. Cambridge Econometrics https://www.camecon.com/wp-content/uploads/2024/03/The-Economic-Burden-of-Long-Covid-in-the-UK_Cambridge-Econometrics_March2024.pdf (March 2024).
-
Fischer, K., Reade, J. J. & Schmal, W. B. What cannot be cured must be endured: the long-lasting effect of a COVID-19 infection on workplace productivity. Labour Econ. 79, 102281 (2022).
Google Scholar
-
Wolff Sagy, Y., Feldhamer, I., Brammli-Greenberg, S. & Lavie, G. Estimating the economic burden of long-COVID: the additive cost of healthcare utilisation among COVID-19 recoverees in Israel. BMJ Glob. Health 8, e012588 (2023).
Google Scholar
-
Ziauddeen, N., Pantelic, M., O’Hara, M. E., Hastie, C. & Alwan, N. A. Impact of long COVID-19 on work: a co-produced survey. Lancet 402, S98 (2023).
-
Perlis, R. H. et al. Association of post–COVID-19 condition symptoms and employment status. JAMA Netw. Open 6, e2256152 (2023).
Google Scholar
-
Ayoubkhani, D. et al. Employment outcomes of people with Long Covid symptoms: community-based cohort study. Eur. J. Public Health 34, 489–496 (2024).
Google Scholar
-
Packard, S. E. & Susser, E. Association of long COVID with housing insecurity in the United States, 2022–2023. SSM Popul. Health 25, 101586 (2024).
Google Scholar
-
Bach, K. New data shows Long COVID is keeping as many as 4 million people out of work. Brookings https://www.brookings.edu/articles/new-data-shows-long-covid-is-keeping-as-many-as-4-million-people-out-of-work/ (24 August 2022).
-
Ham, D. Long-haulers and labor market outcomes. Federal Reserve Bank of Minneapolis https://www.minneapolisfed.org/research/institute-working-papers/long-haulers-and-labor-market-outcomes (7 July 2022).
-
Trades Union Congress. Workers’ experiences of Long Covid. A TUC report. TUC https://www.tuc.org.uk/research-analysis/reports/workers-experience-long-covid (27 March 2023).
-
Ramos, S. C., Maldonado, J. E., Vandeplas, A & Ványolós, I. Long COVID: a tentative assessment of its impact on labour market participation and potential economic effects in the EU. In ECONOMIC BRIEF 077 (European Commission Directorate-General for Economic and Financial Affairs, 2024).
-
Gonzalez, A. E. & Suzuki, E. The impacts of long COVID across OECD countries. OECD Health Working Papers 167 (OECD Publishing, 2024).
-
Baxa, M. An incomplete picture: understanding the burden of long COVID. The Economist Impact https://impact.economist.com/perspectives/sites/default/files/download/ei264_-_an_incomplete_picture_understanding_the_burden_of_long_covid_v8.pdf (29 April 2024).
-
Yuan, H. et al. Progress towards the Sustainable Development Goals has been slowed by indirect effects of the COVID-19 pandemic. Commun. Earth Environ. 4, 184 (2023).
Google Scholar
-
Luyckx, V. A. et al. Sustainable Development Goals relevant to kidney health: an update on progress. Nat. Rev. Nephrol. 17, 15–32 (2021).
Google Scholar
-
Azar, K. M. J. et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 39, 1253–1262 (2020).
-
Martín-Blanco, C., Zamorano, M., Lizárraga, C. & Molina-Moreno, V. The impact of COVID-19 on the Sustainable Development Goals: achievements and expectations. Int. J. Environ. Res. Public Health 19, 16266 (2022).
-
Shuai, C. et al. Quantifying the impacts of COVID-19 on Sustainable Development Goals using machine learning models. Fundam. Res. https://doi.org/10.1016/j.fmre.2022.06.016 (2022).
-
Luyckx, V. A. & Al-Aly, Z. Impact of COVID-19 on the Sustainable Development Agenda and Global Kidney Health. J. Am. Soc. Nephrol. 34, 941–943 (2023).
Google Scholar
-
Ameli, M., Shams Esfandabadi, Z., Sadeghi, S., Ranjbari, M. & Zanetti, M. C. COVID-19 and Sustainable Development Goals (SDGs): scenario analysis through fuzzy cognitive map modeling. Gondwana Res. 114, 138–155 (2023).
Google Scholar
-
Zhang, S., Anser, M. K., Yao-Ping Peng, M. & Chen, C. Visualizing the sustainable development goals and natural resource utilization for green economic recovery after COVID-19 pandemic. Resour. Policy 80, 103182 (2023).
Google Scholar
-
Zhao, W. et al. Achieving the Sustainable Development Goals in the post-pandemic era. Humanit. Soc. Sci. Commun. 9, 258 (2022).
Google Scholar
-
Lukkahatai, N., Rodney, T., Ling, C., Daniel, B. & Han, H. R. Long COVID in the context of social determinants of health. Front. Public Health 11, 1098443 (2023).
Google Scholar
-
Berger, Z., Altiery, D. E. J. V., Assoumou, S. A. & Greenhalgh, T. Long COVID and health inequities: the role of primary care. Milbank Q 99, 519–541 (2021).
Google Scholar
-
Perry, B. L., Aronson, B. & Pescosolido, B. A. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proc. Natl Acad. Sci. USA 118, e2020685118 (2021).
Google Scholar
-
Devoto, S. A. Long COVID and chronic pain: overlapping racial inequalities. Disabil. Soc. 38, 524–529 (2023).
Google Scholar
-
Al-Aly, Z. Prevention of long COVID: progress and challenges. Lancet Infect. Dis. 23, 776–777 (2023).
Google Scholar
-
Au, L., Capotescu, C., Curi, A., Gonçalves Leonel da Silva, R. & Eyal, G. Long COVID requires a global response centred on equity and dialogue. Glob. Health Action 16, 2244757 (2023).
Google Scholar
-
McCorkell, L., Assaf, G, S., Davis, H, E., Wei, H. & Akrami, A. Patient-led research collaborative: embedding patients in the Long COVID narrative. Pain Rep. 6, e913 (2021).
-
Alwan, N. A. The road to addressing Long Covid. Science 373, 491–493 (2021).
Google Scholar
-
Couzin-Frankel, J. & Vogel, G. Vaccines may cause rare, Long Covid-like symptoms. Science 375, 364–366 (2022).
Google Scholar
-
Hofer, U. Animal model of long COVID? Nat. Rev. Microbiol. 20, 446 (2022).
-
Silva, J. et al. Sex differences in symptomatology and immune profiles of Long COVID. Preprint at medRxiv https://doi.org/10.1101/2024.02.29.24303568 (2024).
-
Lammi, V. et al. Genome-wide association study of Long COVID. Preprint at medRxiv https://doi.org/10.1101/2023.06.29.23292056 (2023).
-
Lee, Y. et al. EWAS of post-COVID-19 patients shows methylation differences in the immune-response associated gene, IFI44L, three months after COVID-19 infection. Sci. Rep. 12, 11478 (2022).
Google Scholar
-
Ozturkler, Z. & Kalkan, R. A new perspective of COVID-19 infection: an epigenetics point of view. Glob. Med. Genet. 9, 4–6 (2022).
Google Scholar
-
Wang, R. et al. SARS-CoV-2 restructures host chromatin architecture. Nat. Microbiol. 8, 679–694 (2023).
Google Scholar
-
Gatmaitan, B. G., Chason, J. L. & Lerner, A. M. Augmentation of the virulence of murine coxsackie-virus B-3 myocardiopathy by exercise. J. Exp. Med. 131, 1121–1136 (1970).
Google Scholar
-
van Rhijn-Brouwer, F. C. C. et al. Graded exercise therapy should not be recommended for patients with post-exertional malaise. Nat. Rev. Cardiol. 21, 430–431 (2024).
Google Scholar
-
Xie, Y., Choi, T. & Al-Aly, Z. Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study. Lancet Infect. Dis. 24, 239–255 (2024).
Google Scholar
-
Spinney, L. Pandemics disable people—the history lesson that policymakers ignore. Nature 602, 383–385 (2022).
Google Scholar
-
Spinney, L. Pale Rider: The Spanish Flu of 1918 and How it Changed the World (PublicAffairs, 2017).
-
Bjornevik, K. et al. Longitudinal analysis reveals high prevalence of Epstein–Barr virus associated with multiple sclerosis. Science 375, 296–301 (2022).
Google Scholar
-
Stefano, G. B. Historical insight into infections and disorders associated with neurological and psychiatric sequelae similar to Long COVID. Med. Sci. Monit. 27, e931447 (2021).
Google Scholar
-
Vahratian A., Lin, J. -M. S., Bertolli J. & Unger E. R. Myalgic encephalomyelitis/chronic fatigue syndrome in adults: United States, 2021–2022. NCHS Data Brief 488, 1–6 (2023).
-
Komaroff, A. L. Advances in understanding the pathophysiology of chronic fatigue syndrome. J. Am. Med. Assoc. 322, 499–500 (2019).
Google Scholar
-
Paul, B. D., Lemle, M. D., Komaroff, A. L. & Snyder, S. H. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc. Natl Acad. Sci. USA 118, e2024358118 (2021).
Google Scholar
-
Steiner, S. et al. Understanding, diagnosing, and treating myalgic encephalomyelitis/chronic fatigue syndrome – state of the art: Report of the 2nd International Meeting at the Charite Fatigue Center. Autoimmun. Rev. 22, 103452 (2023).
Google Scholar
-
Arron, H. E. et al. Myalgic encephalomyelitis/chronic fatigue syndrome: the biology of a neglected disease. Front. Immunol. 15, 1386607 (2024).
Google Scholar
-
Goldenberg, D. L. How to understand the overlap of long COVID, chronic fatigue syndrome/myalgic encephalomyelitis, fibromyalgia and irritable bowel syndromes. Semin. Arthritis Rheum. 67, 152455 (2024).
-
Arun, S., Storan, A. & Myers, B. Mast cell activation syndrome and the link with long COVID. Br. J. Hosp. Med. 83, 1–10 (2022).
-
Salvucci, F. et al. Antihistamines improve cardiovascular manifestations and other symptoms of long-COVID attributed to mast cell activation. Front. Cardiovasc. Med. 10, 1202696 (2023).
Google Scholar
-
Sumantri, S. & Rengganis, I. Immunological dysfunction and mast cell activation syndrome in long COVID. Asia Pac. Allergy 13, 50–53 (2023).
-
Weinstock, L. B. et al. Mast cell activation symptoms are prevalent in Long-COVID. Int. J. Infect. Dis. 112, 217–226 (2021).
Google Scholar
-
Chadda, K. R., Blakey, E. E., Huang, C. L. & Jeevaratnam, K. Long COVID-19 and postural orthostatic tachycardia syndrome—is dysautonomia to be blamed? Front. Cardiovasc. Med. 9, 860198 (2022).
Google Scholar
-
Finsterer, J. Small fiber neuropathy underlying dysautonomia in COVID-19 and in post-SARS-CoV-2 vaccination and long-COVID syndromes. Muscle Nerve 65, E31–E32 (2022).
Google Scholar
-
Margalit, I. & Yahav, D. The potential role of vagus nerve dysfunction and dysautonomia in long COVID. Clin. Microbiol. Infect. 30, 423–427 (2024).
Google Scholar
-
Grist, J. T. et al. Lung abnormalities detected with hyperpolarized 129Xe MRI in patients with long COVID. Radiology 305, 709–717 (2022).
Google Scholar
-
Garcia-Hernandez, R. et al. Mapping microglia and astrocyte activation in vivo using diffusion MRI. Sci. Adv. 8, eabq2923 (2022).
Google Scholar
-
Jacob, L. et al. Conserved meningeal lymphatic drainage circuits in mice and humans. J. Exp. Med. 219, e20220035 (2022).
Google Scholar
-
Ajčević, M. et al. Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI. Sci. Rep. 13, 5808 (2023).
Google Scholar
-
Turner, S., Laubscher, G. J., Khan, M. A., Kell, D. B. & Pretorius, E. Accelerating discovery: a novel flow cytometric method for detecting fibrin(ogen) amyloid microclots using long COVID as a model. Heliyon 9, e19605 (2023).
-
Peluso, M. J. et al. Tissue-based T cell activation and viral RNA persist for up to 2 years after SARS-CoV-2 infection. Sci. Transl. Med. 16, eadk3295 (2024).
Google Scholar
-
Espín, E. et al. Cellular and molecular biomarkers of long COVID: a scoping review. eBioMedicine 91, 104552 (2023).
Google Scholar
-
Lai, Y. J. et al. Biomarkers in long COVID-19: a systematic review. Front. Med. 10, 1085988 (2023).
Google Scholar
-
Su, Y. et al. Multi-omics resolves a sharp disease-state shift between mild and moderate COVID-19. Cell 183, 1479–1495 (2020).
Google Scholar
-
Li, H. et al. Plasma proteomic and metabolomic characterization of COVID-19 survivors 6 months after discharge. Cell Death Dis. 13, 235 (2022).
Google Scholar
-
Rusu, E. C. et al. Towards understanding post-COVID-19 condition: a systematic meta-analysis of transcriptomic alterations with sex-specific insights. Comput. Biol. Med. 175, 108507 (2024).
Google Scholar
-
Gu, X. et al. Probing long COVID through a proteomic lens: a comprehensive two-year longitudinal cohort study of hospitalised survivors. EBioMedicine 98, 104851 (2023).
Google Scholar
-
Iosef, C. et al. Plasma proteome of Long-COVID patients indicates HIF-mediated vasculo-proliferative disease with impact on brain and heart function. J. Transl. Med. 21, 377 (2023).
Google Scholar
-
Liang, X., Wang, Y. & Guo, T. Proteomics approaches to long COVID: status and outlooks. Life Med. 2, 3 (2023).
Google Scholar
-
Saito, S. et al. Metabolomic and immune alterations in long COVID patients with chronic fatigue syndrome. Front. Immunol. 15, 1341843 (2024).
Google Scholar
-
López-Hernández, Y. et al. Untargeted analysis in post-COVID-19 patients reveals dysregulated lipid pathways two years after recovery. Front. Mol. Biosci. 10, 1100486 (2023).
Google Scholar
-
Li, Z. et al. The causal role of gut microbiota in susceptibility of Long COVID: a Mendelian randomization study. Front. Microbiol. 15, 1404673 (2024).
Google Scholar
-
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397, 220–232 (2021).
Google Scholar
-
Al-Aly, Z. Long COVID and its cardiovascular implications: a call to action. Eur. Heart J. 44, 5001–5003 (2023).
Google Scholar
-
Thaweethai, T. et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. J. Am. Med. Assoc. 329, 1934–1946 (2023).
Google Scholar
-
Reese, J. T. et al. Generalisable long COVID subtypes: findings from the NIH N3C and RECOVER programmes. eBioMedicine 87, 104413 (2023).
Google Scholar
-
Zhang, H. et al. Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes. Nat. Med. 29, 226–235 (2023).
Google Scholar
-
Liew, F. et al. Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease. Nat. Immunol. 25, 607–621 (2024).
Google Scholar
-
Matthews, A. A., Danaei, G., Islam, N. & Kurth, T. Target trial emulation: applying principles of randomised trials to observational studies. Br. Med. J. 378, e071108 (2022).
Google Scholar
-
Hernán, M. A., Wang, W. & Leaf, D. E. Target trial emulation: a framework for causal inference from observational data. J. Am. Med. Assoc. 328, 2446–2447 (2022).
Google Scholar
-
Xie, Y., Bowe, B., Maddukuri, G. & Al-Aly, Z. Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with COVID-19 and seasonal influenza: cohort study. Br. Med. J. 371, m4677 (2020).
Google Scholar
-
Xie, Y., Choi, T. & Al-Aly, Z. Risk of death in patients hospitalized for COVID-19 vs seasonal influenza in Fall-Winter 2022–2023. J. Am. Med. Assoc. 329, 1697–1699 (2023).
Google Scholar
-
Xie, Y., Choi, T. & Al-Aly, Z. Mortality in patients hospitalized for COVID-19 vs influenza in Fall-Winter 2023–2024. J. Am. Med. Assoc. 331, 1963–1965 (2024).
Google Scholar
-
The Lancet Infectious Diseases. Where are the long COVID trials? Lancet Infect. Dis. 23, 879 (2023).
-
Fairbank, R. Long COVID still has no cure—so these patients are turning to research. Nature 628, 26–28 (2024).
Google Scholar
-
Alwan, N. A. Lessons from Long COVID: working with patients to design better research. Nat. Rev. Immunol. 22, 201–202 (2022).
Google Scholar
-
Loretelli, C. et al. PD-1 blockade counteracts post-COVID-19 immune abnormalities and stimulates the anti-SARS-CoV-2 immune response. JCI Insight 6, e146701 (2021).
Google Scholar
-
Service, R. F. Bad news for Paxlovid? Resistance may be coming. Science 377, 138–139 (2022).
Google Scholar
-
Iketani, S. et al. Multiple pathways for SARS-CoV-2 resistance to nirmatrelvir. Nature 613, 558–564 (2023).
Google Scholar
-
Duan, Y. et al. Molecular mechanisms of SARS-CoV-2 resistance to nirmatrelvir. Nature 622, 376–382 (2023).
Google Scholar
-
Buchholz, S., Di Meco, E., Balkowiec-Iskra, E. Z., Sepodes, B. & Cavaleri, M. Generating clinical evidence for treatment and prevention options for long COVID. Nat. Med. https://doi.org/10.1038/s41591-024-03031-5 (2024).
-
Mohamed, M. O. & Banerjee, A. Long COVID and cardiovascular disease: a learning health system approach. Nat. Rev. Cardiol. 19, 287–288 (2022).
Google Scholar
-
Alwan, N. A. et al. Long Covid active case finding study protocol: a co-produced community-based pilot within the STIMULATE-ICP study (symptoms, trajectory, inequalities and management: understanding Long-COVID to address and transform existing integrated care pathways). PLoS ONE 18, e0284297 (2023).
Google Scholar
-
Black, R. E. et al. Health and development from preconception to 20 years of age and human capital. Lancet 399, 1730–1740 (2022).
Google Scholar
-
Jin, S. L. et al. Social histories of public health misinformation and infodemics: case studies of four pandemics. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(24)00105-1 (2024).
Google Scholar
-
Ravenholt, R. T. & Foege, W. 1918 influenza, encephalitis lethargica, parkinsonism. Lancet 320, 860–864 (1982).
Google Scholar
-
Honigsbaum, M. & Krishnan, L. Taking pandemic sequelae seriously: from the Russian influenza to COVID-19 long-haulers. Lancet 396, 1389–1391 (2020).
Google Scholar
-
Dehner, G. Howard Phillips, in a time of plague: memories of the ‘Spanish’ flu epidemic of 1918 in South Africa. Soc. Hist. Med. 33, 343–344 (2019).
-
Greenhalgh, T. et al. Masks and respirators for prevention of respiratory infections: a state of the science review. Clin. Microbiol Rev. 37, e0012423 (2024).
Google Scholar
-
Etowa, J. et al. Understanding low vaccine uptake in the context of public health in high-income countries: a scoping review. Vaccines 12, 269 (2024).
Google Scholar
-
World Health Organization. Indoor airborne risk assessment in the context of SARS-CoV-2: description of airborne transmission mechanism and method to develop a new standardized model for risk assessment. https://iris.who.int/handle/10665/376346 (World Health Organization, 2024).
-
Morawska, L. et al. Mandating indoor air quality for public buildings. Science 383, 1418–1420 (2024).
Google Scholar
-
Lewis, D. Indoor air is full of flu and COVID viruses. Will countries clean it up? Nature 615, 206–208 (2023).
Google Scholar
-
Lunderberg, D. M. et al. Assessing residential PM2.5 concentrations and infiltration factors with high spatiotemporal resolution using crowdsourced sensors. Proc. Natl Acad. Sci. USA 120, e2308832120 (2023).
Google Scholar
-
Grippo, A. et al. Indoor air pollution exposure and early childhood development in the Upstate KIDS Study. Environ. Res. 234, 116528 (2023).
Google Scholar
-
Lee, K. K. et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 8, e1427–e1434 (2020).
Google Scholar
-
Pulimeno, M., Piscitelli, P., Colazzo, S., Colao, A. & Miani, A. Indoor air quality at school and students’ performance: Recommendations of the UNESCO Chair on Health Education and Sustainable Development & the Italian Society of Environmental Medicine (SIMA). Health Promot. Perspect. 10, 169–174 (2020).
Google Scholar
-
Topol, E. J. & Iwasaki, A. Operation nasal vaccine—lightning speed to counter COVID-19. Sci. Immunol. 7, eadd9947 (2022).
Google Scholar
-
Nunn, A. The Politics and History of AIDS Treatment in Brazil (Springer, 2008).
-
Grangeiro, A. et al. Forty years of the Brazilian response to HIV: reflections on the need for a programmatic shift and policy as a common good. Cad. Saude Publica 39, e00199423 (2023).
Google Scholar
-
Cheever, L. W., Rich, J. & Adashi, E. Y. The Ryan White HIV/AIDS Program: thirty years of addressing health disparities. J. Health Care Poor Underserved 35, 726–730 (2024).
Google Scholar
-
Goyal, R. et al. The health equity implications of the Health Resources and Services Administration’s Ryan White HIV/AIDS Program. AIDS 38, 1025–1032 (2024).
Google Scholar
-
Patel-Larson, A. et al. Looking back to see forward: multidirectional learning between the US Ryan White HIV/AIDS Program and the US President’s Emergency Plan for AIDS Relief. BMJ Glob. Health 8, e013953 (2024).
Google Scholar
-
de Beaumont Foundation. Poll: Physicians agree Long COVID is a problem but are unprepared to treat it. https://debeaumont.org/wp-content/uploads/2023/03/Long-COVID-Brief.pdf (2023).
-
National Center for Health Statistics Rapid Surveys System. Long COVID. https://www.cdc.gov/nchs/rss/round1/long-covid.html (accessed 1 July 2024).
-
Al-Aly, Z. Addressing Long COVID: Advancing Research and Improving Patient Care. US Senate Committee on Health, Education, Labor and Pensions https://www.help.senate.gov/download/al-aly-testimony?download=1 (18 January 2024).
-
Conroy, M. et al. The advantages of UK Biobank’s open-access strategy for health research. J. Intern. Med. 286, 389–397 (2019).
Google Scholar
-
Helzlsouer, K. J. & Reedy, J. Data sharing for the public good. J. Natl Cancer Inst. 112, 867–868 (2020).
Google Scholar
-
Soriano, J. B., Murthy, S., Marshall, J. C., Relan, P. & Diaz, J. V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 22, e102–e107 (2022).
Google Scholar
-
US Centers for Disease Control. Long COVID or post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/ (accessed 1 July 2024).
-
National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing the long-term effects of COVID-19. NICE https://www.nice.org.uk/guidance/ng188 (accessed 1 July 2024).
-
US Department of Health and Human Services, Office of the Assistant Secretary for Health. National Research Action Plan on Long COVID. covid.gov https://www.covid.gov/sites/default/files/documents/National-Research-Action-Plan-on-Long-COVID-08012022.pdf (August 2022).
-
Appel, K. S. et al. Definition of the Post-COVID syndrome using a symptom-based Post-COVID score in a prospective, multi-center, cross-sectoral cohort of the German National Pandemic Cohort Network (NAPKON). Infection https://doi.org/10.1007/s15010-024-02226-9 (2024).
-
Alwan, N. A. & Johnson, L. Defining long COVID: going back to the start. Med 2, 501–504 (2021).
-
Sivan, M. & Heightman, M. A new professional society for post-COVID condition and other post-viral conditions. Adv. Rehabil. Sci. Pract. 13, https://doi.org/10.1177/27536351241231351 (2024).
-
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Global Health; Forum on Microbial Threats. Toward a Post-Pandemic World: Lessons from COVID-19 for Now and the Future: Proceedings of a Workshop (National Academies Press, 2022).
-
To respond to the threat of avian influenza, look back at lessons learned from COVID-19. Nat. Med. 30, 1507 (2024).
-
Sachs, J. D. et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet 400, 1224–1280 (2022).
Google Scholar
-
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20, 193–205 (2022).
Google Scholar
-
de Oliveira, T. & Tegally, H. Will climate change amplify epidemics and give rise to pandemics? Science 381, eadk4500 (2023).
Google Scholar
-
Marani, M., Katul, G. G., Pan, W. K. & Parolari, A. J. Intensity and frequency of extreme novel epidemics. Proc. Natl Acad. Sci. USA 118, e2105482118 (2021).
Google Scholar
-
Carlson, C. J. et al. Climate change increases cross-species viral transmission risk. Nature 607, 555–562 (2022).
Google Scholar
-
Neumann, G. & Kawaoka, Y. Which virus will cause the next pandemic? Viruses 15, 199 (2023).
Google Scholar
-
Vastag, B. & Mazur, B. Researchers warn covid-19 could cause debilitating long-term illness in some patients. The Washington Post https://www.washingtonpost.com/health/could-covid-19-cause-long-term-chronic-fatigue-and-illness-in-some-patients/2020/05/29/bcd5edb2-a02c-11ea-b5c9-570a91917d8d_story.html (30 May 2020).
-
Lowenstein, F. We need to talk about what coronavirus recoveries look like. The New York Times https://www.nytimes.com/2020/04/13/opinion/coronavirus-recovery.html (13 April 2020).
-
Callard, F. & Perego, E. How and why patients made Long COVID. Soc. Sci. Med 268, 113426 (2021).
Google Scholar
-
Young, E. COVID-19 can last for several months. The Atlantic https://www.theatlantic.com/health/archive/2020/06/covid-19-coronavirus-longterm-symptoms-months/612679/ (4 June 2020).
-
Nemer, M. Post-COVID-19 condition in Canada: what we know, what we don’t know and a framework for action. Office of the Chief Science Advisor of Canada https://science.gc.ca/site/science/sites/default/files/attachments/2023/Post-Covid-Condition_Report-2022.pdf (2022).
-
Duddy, C. et al. Coronavirus: long COVID. House of Commons Library https://researchbriefings.files.parliament.uk/documents/CBP-9112/CBP-9112.pdf (29 February 2024).
-
European Commission. Network of expertise on Long COVID. https://health.ec.europa.eu/non-communicable-diseases/expert-group-public-health/network-expertise-long-covid_en (accessed 26 June 2024).
-
Parliament of Australia. Sick and tired: casting a long shadow. https://www.aph.gov.au/Parliamentary_Business/Committees/House/Health_Aged_Care_and_Sport/LongandrepeatedCOVID/Report (April, 2023).
-
US Senate Committee on Health, Education, Labor, and Pensions. Chairman Bernie Sanders releases Long COVID moonshot legislative proposal. https://www.help.senate.gov/chair/newsroom/press/news-chairman-bernie-sanders-releases-long-covid-moonshot-legislative-proposal (9 April 2024).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Z.A.-A. reports receiving consultation fees from Pfizer. L.M. reports consulting fees from Evidera. L.S. has received honoraria from consulting for Evidera. A.I. co-founded RIGImmune, Xanadu Bio and PanV and is a member of the board of directors of Roche Holding and Genentech.
Peer review
Peer review information
Nature Medicine thanks Trisha Greenhalgh, Helen Ward and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article
Al-Aly, Z., Davis, H., McCorkell, L. et al. Long COVID science, research and policy.
Nat Med (2024). https://doi.org/10.1038/s41591-024-03173-6
-
Received: 16 April 2024
-
Accepted: 02 July 2024
-
Published: 09 August 2024
-
DOI: https://doi.org/10.1038/s41591-024-03173-6