Abstract
Some studies have identified influencing factors of COVID-19 illness in elderly, such as underlying diseases, but research on the effect of nutritional status is still lacking. This study retrospectively examined the influence of nutritional status on the outcome of elderly COVID-19 inpatients. A retrospective analysis of the clinical data of 4241 COVID-19 patients who were admitted to a third-class hospital of Nanchang between November 1, 2022 and January 31, 2023 was conducted. Nutritional status was assessed using the prognostic nutritional index (PNI) and controlling nutritional status score (CONUT). The influence of nutritional status on the outcome of COVID-19 patients was determined through multivariate adjustment analysis, restrictive cubic spline, and receiver operating characteristic curve (ROC). Compared with mild/no malnutrition, severe malnutrition substantially increased the critical outcome of COVID-19. A linear relationship was observed between the odds ratio (OR) and PNI and CONUT (P > 0.05). The area under the ROC curve indicated that PNI was the better predictor. The optimal cutoff value of PNI was 38.04 (95%CI: 0.797 ~ 0.836, AUC = 0.817), with a sensitivity of 70.7% and a specificity of 79.6%. The critical illness of elderly COVID-19 patients shows a linear relationship with malnutrition at admission. The use of PNI to assess the prognosis of COVID-19 eldeely patients is reliable, highlighting the importance for doctors to closely pay attention to the nutritional status of COVID-19 patients. Focusing on nutritional status in clinical practice can effectively reduce the critical illness of elderly COVID-19 patients.
Introduction
Corona Virus Disease 2019 (COVID-19) is the third fatal coronavirus infection of the 21st century, which is significantly more lethal than the previous Severe Acute Respiratory Syndromes (SARS) and Middle East respiratory syndrome1. The World Health Organization reported 29.37 million new cases confirmed in the third week of December, 20222. As of May 3, 2023, the global count of confirmed cases has exceeded 760 million, with over 6.92 million deaths.2 Due to the high infectivity and high case fatality rate of COVID-19, people throughout the world are affected by the pandemic. COVID-19 has now become a major public health problem.
Studies have demonstrated an association between nutritional status and mortality from COVID-19 infection3. Malnutrition is an risk factor that negatively affects the clinical outcomes of patients, being associated with an increased risk of adverse events, increased hospital stay and higher mortality, especially in elderly people4. However, there is no clinically clear screening tool for the nutritional status of COVID-19.
The use of a blood-based objective malnutrition index can overcome the limitations of subjective malnutrition screening tools. The prognostic nutritional index (PNI) and controlling nutritional status score (CONUT) can be computed based on three conventional blood parameters: peripheral blood lymphocytes, serum albumin, and total cholesterol. Originally employed to evaluate surgical risk and predict the nutritional and immune status of surgical patients5, other studies have found a correlation between PNI and CONUT and the prognosis of patients with malignant tumors and heart failure6,7.
Therefore, this study retrospectively explores the the influence of nutritional status on the outcome of elderly COVID-19 patients based on PNI and CONUT, while investigating the value of PNI and CONUT in predicting elderly COVID-19 hospital new outcomes. Meanwhile, this study will provide reference opinions for clinicians to assess the nutritional status of COVID-19 patients and help reduce the poor prognosis of elderly COVID-19 patients.
Methods
Data source
In this single-center retrospective study, we obtained data from the Big Data Center Information Management System of a third-class hospital. We collected information and hospital new outcomes on patient sex, age, admission time, underlying disease, surgical status, hospital duration, hospitalization details, discharge outcome, medical records and so on. In addition, laboratory test data, including serum albumin levels and total lymphocyte counts from the first test after admission, were included.
Filters for patient selection included the following criteria: ① Patients diagnosed with novel coronavirus first infection during hospitalization from November 1, 2022, to January 31, 2023; ② According to the COVID-19 Diagnosis and Treatment Protocol (Trial Ninth Edition), patients were confirmed as COVID-19;③ Age ≥ 60 years old. Exclusion criteria: ① Long-term inpatients who were admitted before November 2022; ② Patients with severe loss of clinical data or laboratory diagnostic data; ③ Patients with extremely abnormal clinical data or laboratory diagnostic data; ④ Patients who were still not discharged as of the statistical date (January 31, 2023); ⑤ Patients who are not first-time infected. ⑥Patients who potentially have clinical conditions that alter serum albumin, total lymphocyte count, and total cholesterol, such as the use of statins, patients with advanced liver disease, or patients with lymphoma/leukemia, excluded.
This study included COVID-19 patients admitted to the Second Affiliated Hospital of Nanchang University from November 1, 2022, to January 31, 2023. After applying the Not Applicable (Na) exclusion criteria to exclude duplicate and incomplete information cases, 4241 patients were finally included for retrospective analysis.
This study has been approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University.
Malnutrition screening tools
Patients were screened for malnutrition employing PNI and CONUT. The CONUT score was computed based on serum albumin level, total cholesterol, and lymphocyte count, with scores of 0 to 1 classified as no malnutrition, 2–4, 5–8, and 9–12 indicating mild, moderate, and severe malnutrition, respectively. The PNI score was computed using the formula PNI = serum albumin (g/L) + 5 total lymphocyte count (109/L), with scores > 38 considered free of malnutrition, 35–38 and < 35 representing moderate and severe malnutrition, see Table A1 in Appendix A.
Study cohort
According to the fifth edition of the National Health Council COVID-19 management guidelines, the severity of inpatient outcomes in hospitalized COVID-19 patients was defined. Patients that exhibited any of the following characteristics were considered critical: respiratory failure requiring mechanical ventilation, shock, organ dysfunction, or the need for admission to the intensive care unit.
According to the above standards, patients were classified as “hazardous” and “noncritical” in this study.
Statistical treatment
We employed Python version 3.7 and R version 3.6.3 statistical software for statistical processing. In addition, we expressed the data with a normal distribution as mean ± standard deviation (x ± s) and performed two independent sample t-tests to compare groups. Continuous variables that did not follow a normal distribution were expressed as median and interquartile spacing [M (Q1, Q3)], and the groups were compared using the Mann–Whitney U test. Categorical variables were expressed as frequency (%) and comparison between groups was performed using the χ2 test.
According to the in-hospital outcome, we conducted a univariate analysis of the basic characteristics of COVID-19 patients with different outcomes, multi-model multivariate adjustment analysis, and restricted cubic spline comparative analysis to clarify the impact of nutritional status on the outcome of COVID-19 patients. In the multivariate regression analysis model, the variables were selectively included. In Model 1, only nutrition was included without adjusting for other factors, while age and sex were adjusted in Model 2. Model 3 included all other univariate analysis of meaningful variables. Furthermore, we assessed the highest predictive value according to the subject characteristic (ROC) curve. Restricted cubic spline regression (RCS) was used to flexibly model and visualize the nonlinear relationship between PNI/CONUT and COVID-19 critical hospitalization outcome. All hypothesis tests considered two-sided p<0.05 as a statistically significant difference.
Results
Baseline characteristics
This study included 4241 hospitalized COVID-19 patients, 2507 (59.1%) were male, the mean age of the patients was 67 years and the median hospital stay was 9 days, with 437 (10.3%) in the critical group.The findings demonstrated that compared with the noncritically ill group, the critically ill group exhibited older age, and the differences in the proportion of men, the proportion of combined underlying diseases, and the proportion of surgeries were all statistically significant (p<0.05). Additionally, the PNI scores were significantly lower while the CONUT scores were higher in the critical group than in the noncritical group(Table 1).
Laboratory tests
The findings of the first laboratory test demonstrated lower levels of red blood cell count, lymphocyte count, platelet count, total protein, albumin, hemoglobin, and total cholesterol, while higher levels of sodium, potassium, chloride, white blood cell count, neutrophil count, total bilirubin, creatinine, and lactate dehydrogenase were observed. These differences between the two groups were statistically significant (p<0.05)(Table 2).
Multivariate analysis
In Model 1, only nutrition was included without adjusting for other factors, while age and sex were adjusted in Model 2. Model 3 included surgical treatment, underlying disease, sodium, potassium, chlorine, hemoglobin, red cell count, white cell count, platelet count, neutrophil count, total protein, total bilirubin, creatinine, and lactate dehydrogenase. The findings demonstrated that severe malnutrition, as indicated by PNI (adjusted odds ratio (OR) 4.07,95%CI = 2.79–5.92) and CONUT (adjusted OR 10.00,95%CI = 4.54–22.01), was a significant factor in the multivariate analysis(Table 3).
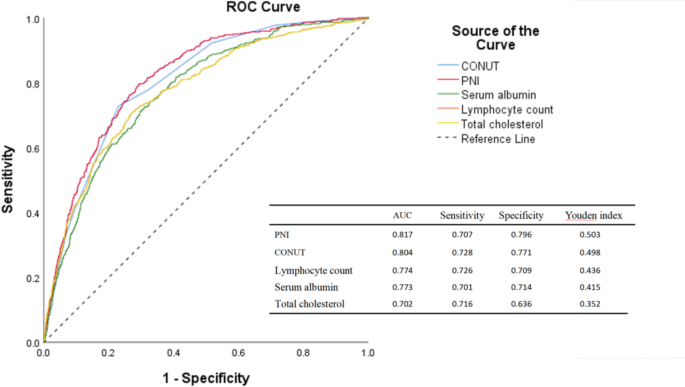
PNI, CONUT, and their independent risk factors
We investigated the ability of PNI, CONUT, and each of its components (serum albumin, total cholesterol, and total lymphocyte count) to predict COVID-19 outcomes using the area under the ROC curve (AUC). The AUCs for PNI, CONUT, serum albumin, total cholesterol, and total lymphocyte counts were 0.817, 0.804, 0.773, 0.702, and 0.774, respectively (Fig. 1). Notably, the AUC of PNI was significantly higher than that of the other four components, and a PNI < 38.04 was the best threshold for predicting critical outcomes in COVID-19 inpatients, with a sensitivity of 70.7% and a specificity of 79.6%.

ROC curves of PNI and CONUT and their components for predicting critical illness.
Restrictive cubic splines of PNI and CONUT
A restrictive cubic spline was conducted to further investigate the association between the two nutritional scores (considered as continuous variables) and inpatient outcomes of COVID-19.The findings indicated a linear relationship between the OR of PNI and CONUT (with P-values of 0.207 and 0.171, respectively). There was a negative dose-response relationship between PNI and COVID-19 critical hospitalization outcome, showing a trend of rapid decline first and then slow decline, that is, the higher the PNI level, the lower the risk of critical hospitalization outcome. A positive dose-response relationship was observed between CONUT and COVID-19 critical hospitalization outcome, with a trend of slow rise first and then rapid rise, that is, the higher the CONUT level, the higher the risk of critical hospitalization outcome. This trend is continuous throughout the range, with no apparent turns.At the reference point (OR = 1), PNI was 40.72 and CONUT was 6, respectively(Fig. 2).
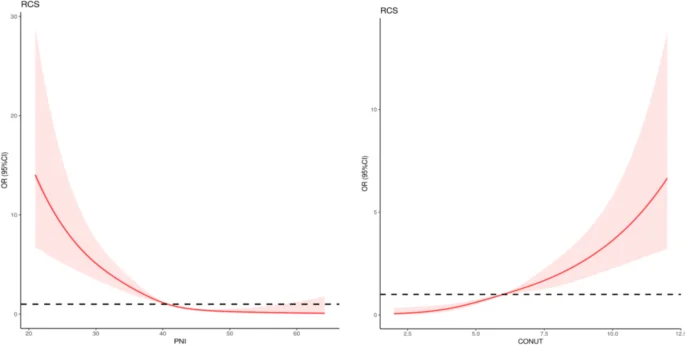
Restrictive cubic spline between PNI, CONUT, and hospital outcomes. Notes: The odds ratio (OR) is represented by the red solid line, and the 95% confidence interval (CI) by the red shaded area.
Discussion
In this study, the critically ill patients were older compared with the noncritically ill group, aligning with similar observations in the US, Saudi Arabia, and Japan8,9,10. This correlation may be attributed to the age-related decline in the function of immune system caused by immune senescence. Moreover, males have higher rates of critical illness because of weaker immunity in these patients11. The reduced female susceptibility to viral infection can be attributed to protection from the X chromosome and sex hormones, which play an important role in both innate and adaptive immunity12. Nutrition is a factor that determines the immune response and can strongly influence the infection trajectory by improving or inhibiting the immune system13. Maintaining good nutrition is crucial for supporting the immune response14. In this study, approximately 34.5% of hospitalized patients in this study showed malnutrition, which is similar to the conclusion reached in the study by Lucie Allard et al. (38.9% of COVID-19 inpatients reported malnutrition).15 The critically ill group exhibited a more unfavorable nutritional status compared with the noncritical group, and it was observed that nutritional risk was associated with severe COVID-19, probably as both a cause and outcome15.
The etiology of malnutrition is complex and multifactorial. Malnutrition associated with disease or injury typically comprises reduced food intake or assimilation and varying degrees of acute or chronic inflammation, leading to changes in body composition and decreased biological function16,17,18. In COVID-19 patients, the origin of malnutrition may be due to reduced food intake, increased digestive and skin loss (diarrhea, vomiting, sweating), olfactory and taste dysfunction, and high catabolism, resulting from high levels of inflammation and muscle atrophy19. When SARS-CoV-2 infects the respiratory tract, it can lead to mild respiratory infection or severe ARS, which triggers an inflammatory response20. Excessive inflammation, cytokine storms, acute respiratory distress syndrome, and damage to the lungs, heart, and kidneys characterize severe COVID-193. Huang et al. discovered that SARS-CoV-2 attacked the mucosal epithelium, resulting in gastrointestinal symptoms and worsening the nutritional status of elderly patients21. What’s more, the development of malnutrition in the elderly is also most likely facilitated by the aging process22.
Insufficient nutrition due to malnutrition may lead to inflammation, oxidative stress disorders and inadequate availability of optimal functioning immune system, resulting in increased susceptibility to infection and inability to control infection, ultimately leading to adverse consequences such as frailty and infection23.Malnutrition in the elderly presents with involuntary weight loss or low body mass index, and a higher risk of malnutrition is associated with decreased muscle mass at admission in elderly inpatients24. The reduction in lean body mass usually represents no metabolic reserve in the elderly. In addition to undernutrition, overnutrition, represented by obesity and overweight, constitutes adverse factors for novel coronavirus infection in older patients, and a higher Body Mass Index (BMI) in older patients is associated with negative COVID-19 outcomes23.
According to the laboratory test results, the critically ill COVID-19 inpatients had lower serum albumin, total cholesterol, and lymphocyte values. Serum albumin, particularly in Chinese elderly individuals, serves as an indicator of nutritional status25. Hypoalbuminaemia is closely associated with adverse clinical outcomes26. In severe COVID-19 patients, SARS-CoV-2 may not only trigger an antiviral immune response, but may also lead to excessive production of proinflammatory cytokines, leading to an uncontrolled inflammatory response. This condition can result in lymphopenia and lymphocyte dysfunction, rendering patients more susceptible to infection, septic shock, and severe multiorgan dysfunction27. Lymphopenia is a crucial factor in disease severity and is a characteristic feature of severe COVID-1928.
In this study, the AUC value of PNI was higher than that of CONUT, serum albumin, total cholesterol, and lymphocytes, which had a good predictive value for the prognosis of patients hospitalized with COVID-19. Low PNI was an independent risk factor for critical inpatient outcome in COVID-19 patients and had a positive dose-response relationship with the risk of critical outcome. This is in line with the findings of shang et al., who showed a monotonic decline trend of 90-day all-cause mortality risk in patients with spontaneous ICH with increasing PNI levels29. PNI, reflecting the intersection of nutritional and inflammatory statuses, may provide more accurate predictive values for adverse outcomes compared to other nutritional scores30. Therefore, PNI is a reliable predictor to adverse the prognosis of COVID-19 elderly patients.
The Global Leadership Initiative on Malnutrition (GLIM) have noted that once malnutrition is diagnosed, skeletal muscle function should be investigated as a relevant component of sarcopenia and for complete nutrition assessment of persons with malnutrition31. The role of micronutrients in supporting the immune system has been widely investigated32,33. Existing evidence indicates that supplementing multiple micronutrients with immune-supporting effects can modulate immune function and mitigate the risk of infection32. Early nutritional management can lead to recovery from malnutrition after COVID-19 hospitalization19. Considering that the mean delay between the first onset of symptoms and admission is about one week, this observation suggests that nutritional support should be provided to each COVID-19 patient before admission. In addition, doctors should focus on nutritional status in clinical practice.early nutritional support for patients with high nutritional risk can effectively reduce the incidence of critical illness15.
This study is characterized by a large sample size, a large amount of data, and high confidence. However, this study also presents some limitations, such as: (1) The samples are solely from one hospital, resulting in a potential single-center bias; (2) This study lacks external validation due to the availability of the data; (3) Since clinical treatment did not explicitly perform standardized nutritional intervention, this retrospective study lacks nutritional intervention and pre-post comparison for malnourished patients; (4) The types of laboratory test data are limited, and the research is not comprehensive; (5) In this study, the linear relationship may limit the power of the restrictive cubic spline in revealing potential non-linear features between PNI and COVID-19 prognosis. Therefore, the results of this study may not fully reflect the complex relationships between the variables.Future studies could attempt to combine restrictive cubic splines with other nonlinear methods to form a more powerful analytical framework to improve model prediction and interpretation capabilities.
Conclusion
In conclusion, the critical illness of elderly COVID-19 patients shows a linear relationship with malnutrition at admission. PNI is a highly valuable biomarker independently associated with elderly COVID-19 severity, and the inpatient outcome of elderly COVID-19 hospitalized patients with PNI < 38.04 may be critical. Future studies are warranted to explore nutritional intervention treatment and pre-post comparison for malnourished elderly COVID-19 hospitalized patients, as well as external and internal validities.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
-
Čivljak, R., Markotić, A. & Kuzman, I. The third coronavirus epidemic in the third millennium: what’s next? Croat Med. J. 61 (1), 1–4 (2020).
Google Scholar
-
WHO Coronavirus Disease (COVID-19. ) Dashboard -World Health Organization.www.who.int.Accessed16/3/2023.
-
da Silva, C. L. et al. Nutritional factors associated with mortality in hospitalized patients with COVID-19. Clin. Nutr. Open. Sci. 45, 17–26 (2022).
Google Scholar
-
Xie, H. et al. The inflammatory burden index is a superior systemic inflammation biomarker for the prognosis of non-small cell lung cancer. J. Cachexia Sarcopenia Muscle. 14 (2), 869–878 (2023).
Google Scholar
-
Wang, Z. et al. Pretreatment prognostic nutritional index as a prognostic factor in lung cancer: review and meta-analysis. Clin. Chim. Acta. 486, 303–310 (2018).
Google Scholar
-
Hao, J. et al. Prognostic value of Pre-treatment Prognostic Nutritional Index in Esophageal Cancer: a systematic review and Meta-analysis. Front. Oncol. 10, 797 (2020).
Google Scholar
-
Chen, M. Y. et al. Association between Prognostic Nutritional Index and Prognosis in patients with heart failure: a Meta-analysis. Front. Cardiovasc. Med. 9, 918566 (2022).
Google Scholar
-
Gold, J. A. W. et al. Race, ethnicity, and Age trends in persons who died from COVID-19 – United States, May-August 2020. MMWR Morb Mortal. Wkly. Rep. 69 (42), 1517–1521 (2020).
Google Scholar
-
Ibrahim, M. E., Al-Aklobi, O. S., Abomughaid, M. M. & Al-Ghamdi, M. A. Epidemiological, clinical, and laboratory findings for patients of different age groups with confirmed coronavirus disease 2019 (COVID-19) in a hospital in Saudi Arabia. PLoS One. 16 (4), e0250955 (2021).
Google Scholar
-
Asai, Y. et al. Comorbidities as risk factors for severe Disease in Hospitalized Elderly COVID-19 patients by different age-groups in Japan. Gerontology. 68 (9), 1027–1037 (2022).
Google Scholar
-
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 395 (10223), 507–513 (2020).
Google Scholar
-
Jaillon, S., Berthenet, K. & Garlanda, C. Sexual dimorphism in Innate Immunity. Clin. Rev. Allergy Immunol. 56 (3), 308–321 (2019).
Google Scholar
-
Moallemian Isfahani, M., Emam-Djomeh, Z., Rao, I. M. & Rezaei, N. Nutrition and Immunity in COVID-19. Adv. Exp. Med. Biol. 1318, 485–497 (2021).
Google Scholar
-
Calder, P. C. Nutrition and immunity: lessons for COVID-19. Nutr. Diabetes. 11 (1), 19 (2021).
Google Scholar
-
Allard, L. et al. Malnutrition: Percentage and Association with prognosis in patients hospitalized for Coronavirus Disease 2019. Nutrients. 12 (12), 3679 (2020).
Google Scholar
-
Hegazi, R., Miller, A. & Sauer, A. Evolution of the diagnosis of malnutrition in adults: a primer for clinicians. Front. Nutr. 11, 1169538 (2024).
Google Scholar
-
Krznarić, Ž. et al. Clinical nutrition in primary care: ESPEN position paper. Clin. Nutr. 21, S0261. 5614 (24) 00059 – 1 (2024).
-
Muscaritoli, M. et al. Disease-related malnutrition with inflammation and cachexia. Clin. Nutr. 42 (8), 1475–1479 (2023).
Google Scholar
-
Bedock, D. et al. Evolution of Nutritional Status after Early Nutritional Management in COVID-19 hospitalized patients. Nutrients. 13 (7), 2276 (2021).
Google Scholar
-
Zabetakis, I., Lordan, R., Norton, C. & Tsoupras, A. COVID-19: the inflammation link and the role of Nutrition in potential mitigation. Nutrients. 12 (5), 1466 (2020).
Google Scholar
-
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 395 (10223), 497–506 (2020).
Google Scholar
-
Norman, K., Haß, U. & Pirlich, M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients. 13 (8), 2764 (2021).
Google Scholar
-
de Siqueira, J. V. V. et al. Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review. Obes. Res. Clin. Pract. 14 (5), 398–403 (2020).
-
Pierik, V. D. et al. High risk of malnutrition is associated with low muscle mass in older hospitalized patients – a prospective cohort study. BMC Geriatr. 17 (1), 118 (2017).
Google Scholar
-
Li, A. et al. The effect of urinary essential and non-essential elements on serum albumin: evidence from a community-based study of the elderly in Beijing. Front. Nutr. 9, 946245 (2022).
Google Scholar
-
Park, S. et al. Optimal nutritional support strategy based on the Association between Modified NUTRIC score and 28-Day mortality in critically ill patients: a prospective study. Nutrients. 15 (11), 2465 (2023).
Google Scholar
-
Delshad, M. et al. The contributory role of lymphocyte subsets, pathophysiology of Lymphopenia and its implication as prognostic and therapeutic opportunity in COVID-19. Int. Immunopharmacol. 95, 107586 (2021).
Google Scholar
-
Li, T., Zheng, F. & Cheng, F. The function of myeloid-derived suppressor cells in COVID-19 lymphopenia. Int. Immunopharmacol. 112, 109277 (2022).
Google Scholar
-
Jhang, S. W., Liu, Y. T., Kor, C. T., Wu, Y. P. & Lai, C. H. Low Prognostic Nutritional Index predicts In-Hospital complications and Case Fatality in patients with spontaneous intracerebral hemorrhage: a retrospective study. Nutrients. 16 (12), 1841 (2024).
Google Scholar
-
Xing, L., Xiong, J., Hu, Q., Li, W. & Chen, L. Comparative analysis of four nutritional scores in predicting adverse outcomes in biopsy-confirmed diabetic kidney disease. Front. Nutr. 11, 1352030 (2024).
Google Scholar
-
Barazzoni, R. et al. Guidance for assessment of the muscle mass phenotypic criterion for the Global Leadership Initiative on Malnutrition (GLIM) diagnosis of malnutrition. Clin. Nutr. 41 (6), 1425–1433 (2022).
Google Scholar
-
Gombart, A. F., Pierre, A. & Maggini, S. A review of micronutrients and the Immune System-Working in Harmony to reduce the risk of infection. Nutrients. 12 (1), 236 (2020).
Google Scholar
-
Junaid, K. et al. Effective Immune functions of micronutrients against SARS-CoV-2. Nutrients. 12 (10), 2992 (2020).
Google Scholar
Acknowledgements
We gratefully acknowledge the invaluable contribution of the study participants. This study was supported by the National Natural Science Foundation of China (81960609), the National Key R&D Program of China (2020YFC2002901 and 2018YFC1312902), The Second Affiliated Hospital of Nanchang University Funding Program (2021efyB03). This work is supported by Extreme Smart Analysis platform.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. Research conception and design, analysis, interpretation of data and manuscript drafting were performed by Xiaoman Wang. Acquisition of data were performed by Jingyao Ke, Rui Cheng and Hongfei Xian. Manuscript drafting and supervision were performed by Jingyi Li, Yongsen Chen, Bin Wu, Mengqi Han, Yifan Wu and Weijie Jia. Revision and final approval of the version of the manuscript to be submitted were performed by Pengfei Yu , Jianmo Liu, Haowen Luo and Yingping Yi. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The present study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University. Written informed consent was obtained from all the patients or their guardians.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Reprints and permissions
About this article
Cite this article
Wang, X., Ke, J., Cheng, R. et al. Malnutrition is associated with severe outcome in elderly patients hospitalised with COVID-19.
Sci Rep 14, 24367 (2024). https://doi.org/10.1038/s41598-024-76363-4
-
Received: 03 June 2024
-
Accepted: 14 October 2024
-
Published: 17 October 2024
-
DOI: https://doi.org/10.1038/s41598-024-76363-4
Keywords
- COVID-19
- Elderly people
- Nutritional status
- Prognostic nutritional index
- Controlling nutritional status score
- Retrospective cohort study