Even after the end of the COVID-19 pandemic, nurses are facing burnout and high levels of stress at work as the health care worker shortage continues.
The Hospital and Healthsystem Association of Pennsylvania’s third annual Hospital Workforce Survey shows that most hospitals in the state are taking steps to address the shortage, and some are even making some headway in filling key roles. Yet more work needs to be done.
The United States is in the middle of a health care worker shortage, one that is expected to get worse in the next few years. According to HAP, Pennsylvania won’t experience its overall worst shortage of nurses, and third-worst shortage of nursing support professionals and mental health providers, until 2026.
Last year, average vacancy rates statewide were between 10% and 19% for certified registered nurse practitioners, certified registered nurse anesthetists, registered direct patient care nurses, clinical nurse specialists, nursing support staff and certified nurse midwives.
At the same time, turnover within nursing jobs is high, and industry workforce surveys conducted by AMN Healthcare, a staffing company that specializes in health care, provide more details.
One survey completed in 2024 collected 186 responses from hospital nurse leaders, and one in 2023 collected 18,226 responses from registered nurses.
When registered nurses were asked what they would be doing in the next year, only 40% said they would continue in their current role, while 15% responded that they would seek a new employer, 12% said they would work as travel nurse and 5% said they would leave nursing to work in another field.
When nurse leaders — such as chief nursing officers and executives, directors of nursing and nurse managers — were asked the same thing, 71% said they planned to stay in their current roll but a sizable percentage of respondents also said they would be leaving their jobs. A total of 17% said they would seek a new employer and 9% of nurse leaders said they would leave to work in another field.
According to AMN, the cause of turnover and exodus out of nursing could be attributed to burnout. About 72% of nurse leaders said they sometimes, often or always experience burnout in their jobs, whereas only 28% said they rarely or never do. Meanwhile, more than 8 in 10 RNs said they experience a great deal or a lot of stress at work, and 68% said they either agree or strongly agree with the statement “most days I feel burned out.”
This was up from 2021 when about 65% or RNs said they experienced a great deal or a lot of stress at work and 57% said most days they felt burnt out.
At the same time, HAP noted one positive trend for Pennsylvania: Turnover rates for “key positions” decreased by 28% from 2022 to 2023. This may be due to concerted efforts by hospitals through recruitment and retention efforts.
Jamie Stover, a spokesperson for Lehigh Valley Health Network, said as part of efforts to attract and retain talent, the network offers competitive compensation, benefits and financial support for continued education for career development.
“We routinely survey our 23,000 colleagues to understand what matters most to them so we can continue to evolve our offerings,” Stover said.
Because of this, LVHN recently announced child care offerings for network employees in the Lehigh Valley and it plans to expand those benefits to other regions. She added LVHN has hired over 500 patient care support staff over the last year and that the network is investing in technology to support staffing and is currently reviewing predictive staffing analytics platforms.
St Luke’s University Health Network, which recently hired its 20,000th employee, did not respond to questions by press time.
For HAP’s survey, nearly all respondents reported making recruitment and retention efforts such as increasing base pay for employees, offering flexible work schedules, professional development and tuition reimbursement.
According to AMN’s survey, these methods were among the top ones favored by nurse leaders for retaining nurses. However, according to AMN, nurses leaders also said top methods for retaining nurses included hospitals implementing favorable nurse-to-patient ratios that increase nurse’s time per patient and decrease feelings of being over worked as well as ensuring effective onboarding and orientation process are in place, which AMN defined as how clearly the parameters and expectations of a nurse’s job are communicated.
Hospitals will not be able to address staffing shortages on their own, according to HAP; major investment and collaboration from educators and governments will be essential to changing this trajectory and growing a health care workforce so it can meet Pennsylvania’s needs.
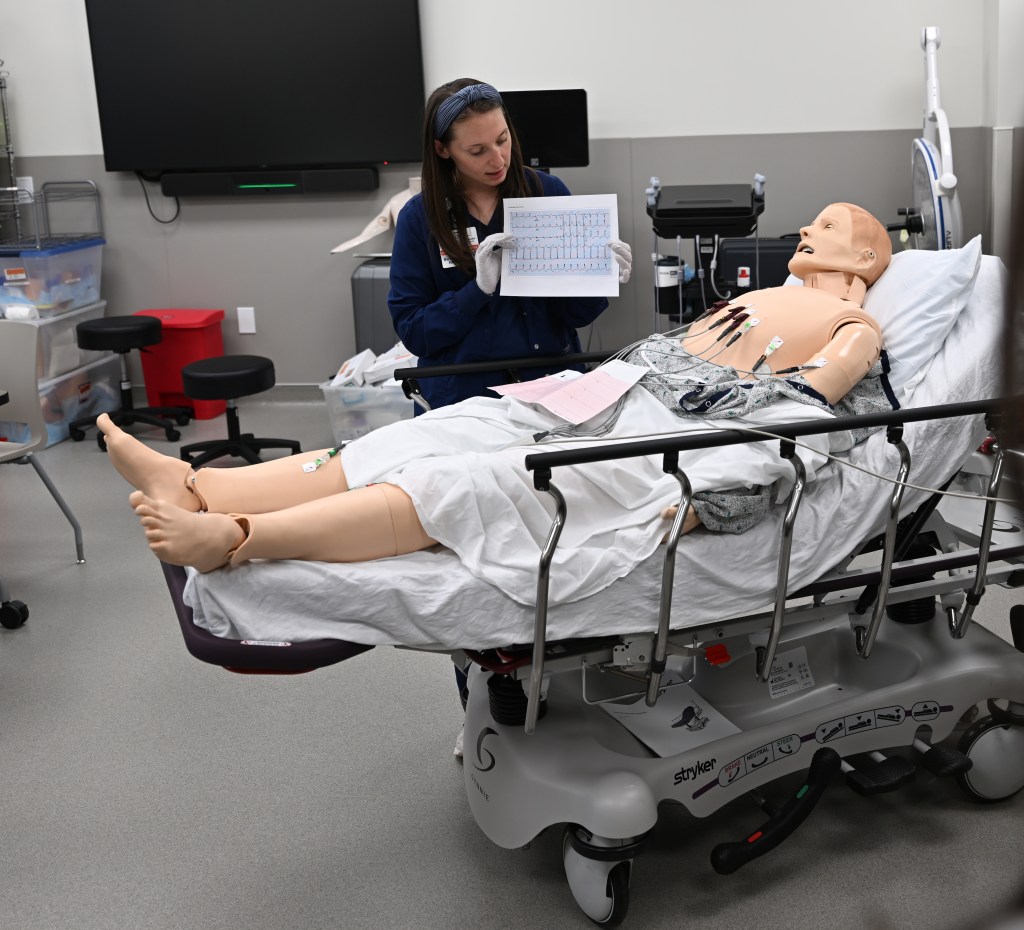
Stover said taking advantage of its own educational programs is part of LVHN’s strategy to improve and grow its workforce. She said the Joseph F. McCloskey School of Nursing is in the process of expanding and will start offering night and weekend classes in Schuylkill County.
“We anticipate offering that same education at our Center for Healthcare Education to accommodate more learners and build a local pipeline for future needs,” Stover said.