There is a public health epidemic of burnout, depression, and suicide in the nursing and healthcare workforce. While the most trusted health profession in the nation does an outstanding job encouraging those suffering from mental health conditions to seek treatment, stigma and other barriers prevent nurses from seeking help when they are struggling.
The Americans With Disabilities Act (ADA) became law in 1990 and serves to protect individuals with physical and mental disabilities from discrimination in numerous facets of life, including employment. Anyone who has completed a job application may recall being asked if they would need any reasonable accommodation to perform their job — this question is the ADA at work. But what frequently gets overlooked is how the ADA applies to professional licensing, such as nurse licensing applications.
Nurse licensing is controlled by individual state boards of nursing (BONs), which collectively form the National Council of State Boards of Nursing (NCSBN). BONs operate to protect the public by regulating the provision of nurse licensing and removal of unsafe clinicians from practice. To flag any potential problems in nurses, BONs have historically defaulted to including what we view as overly invasive questions concerning applicants’ mental health on licensing applications. Often, these questions go beyond inquiries regarding current impairment and request that applicants with a history of mental health disorders detail their related treatment histories, substance use history, breaks in practice, and notarized doctor approvals to practice.
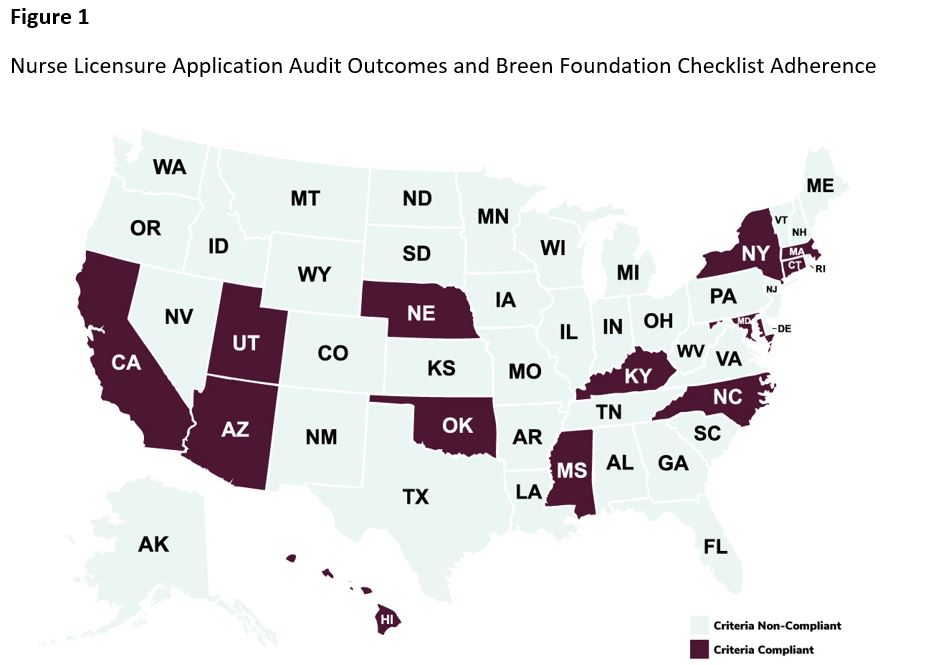
As state entities, BONs are required to adhere to the ADA. Yet, in 2019, a study in the Journal of Psychosocial Nursing and Mental Health Services identified 22 BONs that asked ADA non-compliant questions. More recently, our study in Worldviews on Evidence-Based Nursing used the Dr. Lorna Breen Heroes’ Foundation’s Toolkit to identify BONs with invasive questioning, concluding that 37 states did not meet the Toolkit guidelines for adherence (Figure 1).

Impact on Nurses
While filling out her license renewal application, our peer, Sue Brammer, PhD, RN, came across a question that required her to disclose her bipolar diagnosis and provide treatment documentation.
“When the question appeared about bipolar disorder and I couldn’t proceed in my application unless I provided documentation from my doctors about my treatment for it, I was furious,” Brammer said. “Who would see it, and what qualifications did the person reviewing my doctors’ letters possess to determine whether I was safe? Upon reflection, however, my anger turned to sadness. I was sad for nurses carrying the double burden of managing a mental illness plus the fear of being found out. They won’t seek treatment because they’re afraid of possible repercussions from the Board, and when they don’t get treatment, the suffering can become unbearable and tragic things can happen.”
The mental health crisis in health workers pre-dates the COVID-19 pandemic. However, rapid pandemic-related changes only added fuel to a quickly spreading fire. Between 2018 and 2022, health workers reported an increase of poor mental health days experienced during the previous month (from 3.3 to 4.5 days). A 2022 Surgeon General’s Advisory noted that up to 54% of nurses and physicians are experiencing burnout, which has played a substantial role in our current health worker shortage. Additionally, death by suicide is higher among nurses than the general population, and poor mental health can adversely affect healthcare quality and may play a role in medical errors. In short, our nation’s nurses and health workers are in dire need of support.
A Move in the Right Direction
Approaches to preventing burnout and suicide include decreasing mental health stigma, removing barriers to care, and creating wellness cultures and policies that support clinician well-being. Asking invasive mental health questions on nurse licensing applications supports none of these preventative initiatives. It encourages nurses to withhold information and discourages pursuing care due to a fear of license revocation.
The NCSBN is currently working on national recommendations for the removal of invasive mental health and substance use questions from nurse licensure applications. Until their guidance is released, BONs can look to the Federation of State Medical Boards, the American Medical Association, and the Dr. Lorna Breen Heroes’ Foundation for how to modify invasive questions. These entities recommend either removing questions that enquire about an applicant’s health completely or using language that addresses both physical and mental health with no added asterisks.
For example, “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical, and professional manner?”
State governments have also been working to legally mandate the removal of inappropriate mental health questions across all healthcare professions’ licensing. Virginia’s HB 1573 instructs health regulatory boards within the Department of Health Professions to amend its licensure, certification, and registration applications by removing any existing questions relating to mental health conditions and impairment, and replacing these questions with the following:
- Do you have any reason to believe that you would pose a risk to the safety or well-being of your patients or clients?
- Are you able to perform the essential functions of a practitioner in your area of practice with or without reasonable accommodation?
This Virginia legislation benefits over 500,000 licensed health workers in 62 professions and is quickly becoming a model for other states. For example, similar legislation was signed by the Governor of Illinois in August 2023, but the provisions only apply to the Illinois State Medical Board.
Our Call for Action
The Dr. Lorna Breen Heroes’ Foundation uses an audit, change, and communicate model to advance changes to the invasive mental health questions paradigm. Licensing boards, hospitals, and health systems can become “Well-Being First Champions” that recognize and encourage the removal of probing mental health questions. Twenty-six states have received this designation for medical licensing, and 11 more are actively pursuing it. However, no states are currently Well-Being Champions for nursing licensing. States interested in receiving this designation should submit their Toolkit compliant initial and renewal applications to the Dr. Lorna Breen Heroes’ Foundation. Advocates who wish to invite their BONs to the challenge can contact their state nursing boards. In past weeks, over 75 emails have been sent to BONs in almost every state. By removing these questions, we can remove a major barrier for nurses to seek help for mental health conditions and, hopefully, prevent more nurses from dying by suicide.
Bernadette Mazurek Melnyk, PhD, APRN-CNP, is vice president for Health Promotion and Chief Wellness Officer at Ohio State University in Columbus, as well as the Helene Fuld Health Trust Professor of Evidence-based Practice in the College of Nursing and Professor of Pediatrics and Psychiatry in the College of Medicine at Ohio State. She is an internationally recognized expert, speaker, author, and scientist in the fields of mental health, evidence-based practice, and intervention research. Andreanna Pavan Hsieh, MPH, is an experienced science writer at Ohio State University’s College of Nursing. She applies a public health lens to mental health promotion and champions the prioritization of well-being in the workplace. J. Corey Feist, JD, MBA, is the CEO and co-founder of the Dr. Lorna Breen Heroes’ Foundation. He has over 20 years of experience as a healthcare executive, and is an influential advocate for improving healthcare worker well-being.
Please enable JavaScript to view the comments powered by Disqus.