Hooper L, Bunn D, Jimoh FO, Fairweather-Tait SJ. Water-loss dehydration and aging. Mech Ageing Dev. 2014 Mar-Apr;136–137:50 – 8.
El-Sharkawy AM, Sahota O, Maughan RJ, Lobo DN. The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clin Nutr. 2014;33(1):6–13. Epub 2013 Nov 22. PMID: 24308897.
Google Scholar
Shlisky J, Bloom DE, Beaudreault AR, et al. Nutritional considerations for healthy aging and reduction in age-related chronic disease. Adv Nutr. 2017;8(1):17.
Google Scholar
Tittikpina NK, Issa A-r, Yerima M, et al. Aging and nutrition: theories, consequences, and impact of nutrients. Curr Pharmacol Rep. 2019;5(4):232–43.
Google Scholar
Host A, McMahon A-T, Walton K, Charlton K. Factors influencing food choice for independently living older people—a systematic literature review. J Nutr Gerontol Geriatr. 2016;35(2):67–94.
Google Scholar
Starr KNP, McDonald SR, Bales CW. Nutritional vulnerability in older adults: a continuum of concerns. Curr Nutr Rep. 2015;4(2):176–84. https://doi.org/10.1007/s13668-015-0118-6. /06/01 2015.
Google Scholar
Cardenas D, Correia MITD, Ochoa JB, et al. Clinical nutrition and human rights. An international position paper. Clin Nutr. 2021;40(6):4029–36.
Google Scholar
Holdoway A, Page F, Bauer J, Dervan N, Maier AB. Individualised Nutritional Care for Disease-related malnutrition: improving outcomes by focusing on what matters to patients. Nutrients Aug. 2022;27(17). https://doi.org/10.3390/nu14173534.
Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Goisser S, Hooper L, Kiesswetter E, Maggio M, Raynaud-Simon A, Sieber CC, Sobotka L, van Asselt D, Wirth R, Bischoff SC. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. 2019;38(1):10–47. Epub 2018 Jun 18. PMID: 30005900.
Google Scholar
van Tiel S, Rood PP, Bertoli-Avella AM, et al. Systematic review of frequent users of emergency departments in non-US hospitals: state of the art. Eur J Emerg Med Oct. 2015;22(5):306–15. https://doi.org/10.1097/mej.0000000000000242.
Google Scholar
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS ONE. 2018;13(8):e0203316. https://doi.org/10.1371/journal.pone.0203316.
Google Scholar
Roe L, Thomas S, Trépel D, Normand C. Trends in healthcare cover and healthcare use for older adults in Ireland during the austerity years of 2009–2016. 2018:151. Wellbeing and Health in Ireland’s over 50s 2009–2016.
Griffin A, O’Neill A, O’Connor M, et al. The prevalence of malnutrition and impact on patient outcomes among older adults presenting at an Irish emergency department: a secondary analysis of the OPTI-MEND trial. BMC Geriatr. 2020;20:455. https://doi.org/10.1186/s12877-020-01852-w.
Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-López A, Bueno-Vidales N, Montoro-Huguet M. Malnutrition screening and assessment. Nutrients. 2022;14(12):2392. https://doi.org/10.3390/nu14122392.
Vivanti A, Isenring E, Baumann S, et al. Emergency department malnutrition screening and support model improves outcomes in a pilot randomised controlled trial. Emerg Med J. 2015;32(3):180. https://doi.org/10.1136/emermed-2013-202965.
Google Scholar
Cederholm T, Jensen G, Correia M, et al. GLIM criteria for the diagnosis of malnutrition–A consensus report from the global clinical nutrition community. J cachexia Sarcopenia Muscle. 2019;10(1):207–17.
Google Scholar
Umegaki H, Asai A, Kanda S, et al. Factors associated with unexpected admissions and mortality among low-functioning older patients receiving home medical care. Article Geriatr Gerontol Int. 2017;17(10):1623–7. https://doi.org/10.1111/ggi.12943.
Google Scholar
Swan WI, Vivanti A, Hakel-Smith NA, et al. Nutrition care process and model update: toward realizing people-centered care and outcomes management. J Acad Nutr Dietetics. 2017;117(12):2003–14.
Google Scholar
Swan WI, Pertel DG, Hotson B, et al. Nutrition care process (NCP) update part 2: developing and using the NCP terminology to demonstrate efficacy of nutrition care and related outcomes. J Acad Nutr Dietetics. 2019;119(5):840–55.
Google Scholar
Lövestam E, Steiber A, Vivanti A, et al. Use of the nutrition care process and nutrition care process terminology in an international cohort reported by an online survey tool. J Acad Nutr Dietetics. 2019;119(2):225–41.
Google Scholar
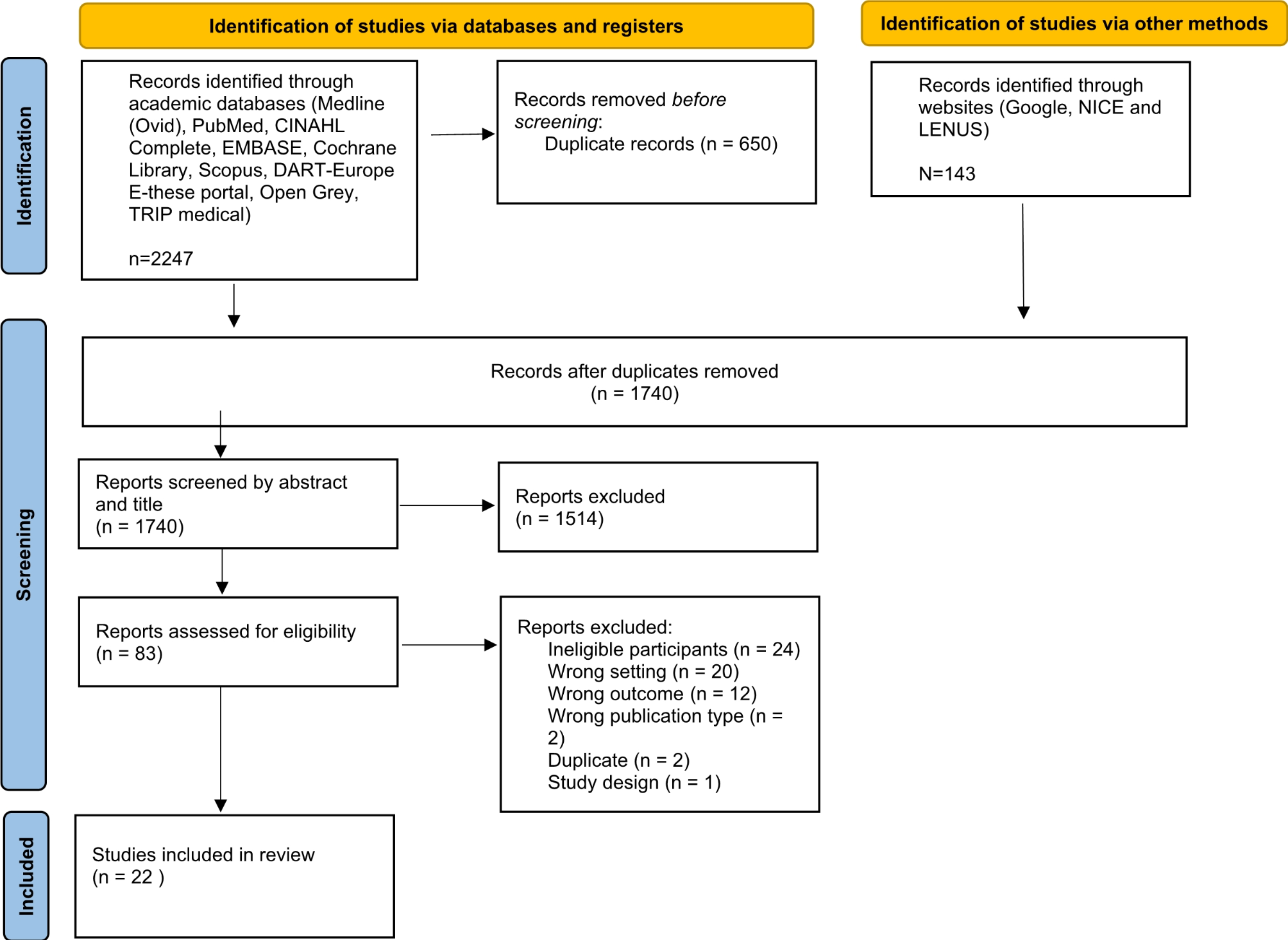
Griffin A, Cerenay S, Ryan L, et al. What is the level of nutrition care provided to older adults attending emergency departments? A scoping review protocol. HRB Open Res. 2022;5:7.
Google Scholar
Peters MD, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthesis. 2020;18(10):2119–26.
Google Scholar
Adams J, Hillier-Brown FC, Moore HJ, et al. Searching and synthesising ‘grey literature’and ‘grey information’in public health: critical reflections on three case studies. Syst Reviews. 2016;5(1):1–11.
Google Scholar
Piasecki J, Waligora M, Dranseika V. Google search as an additional source in systematic reviews. Sci Eng Ethics. 2018;24(2):809–10.
Google Scholar
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Reviews. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4. 12/05 2016.
Google Scholar
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Google Scholar
Li THJ, Deeks JJ,Chapter 5: Collecting data. Cochrane;, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022).
Harfield SG, Davy C, McArthur A, Munn Z, Brown A, Brown N. Characteristics of indigenous primary health care service delivery models: a systematic scoping review. Globalization Health. 2018;14(1):1–11.
Google Scholar
Martín-Sánchez FJ, Triana FC, Rossello X, et al. Effect of risk of malnutrition on 30-day mortality among older patients with acute heart failure in Emergency Departments. Eur J Intern Med. 2019;65:69–77.
Google Scholar
Jiménez CB, Ovalle HF, Moreno MM, de la Fuente RA, de Luis Román D. Undernutrition measured by the Mini Nutritional Assessment (MNA) test and related risk factors in older adults under hospital emergency care. Nutrition. 2019;66:142–6.
Google Scholar
Brady D, Boyle O, Kelly L, et al. 172 Sarcopenia, Frailty and Malnutrition in the older adults in the Emergency Department setting. Volume 48. Age & Ageing; 2019.
O’Caoimh R, Costello M, Small C, et al. Comparison of Frailty Screening instruments in the Emergency Department. Int J Environ Res Public Health. 2019;16(19). https://doi.org/10.3390/ijerph16193626.
Gaffney L, Jonsson A, Judge C, Costello M, O’Donnell J, O’Caoimh R. Using the Surprise question to Predict Frailty and Healthcare outcomes among older adults attending the Emergency Department. Int J Environ Res Public Health. 2022;19(3):1709.
Google Scholar
Muldoon N, Stapleton C, Kane J et al. Frail Elderly Pilot Programme Connolly Hospital Blanchardstown 2016. Int J Integr Care. 2017;17(5).
Stapleton C. Role of the Dietitian within the Frail Elderly Pilot in Connolly Hospital Blanchardstown from February to June 2016. Int J Integr Care (IJIC). 2017;17.
O’Caoimh R. Validation of the risk instrument for screening in the community (RISC) among older adults in the emergency department. Int J Environ Res Public Health. 2023;20(4):3734.
Google Scholar
Burks CE, Jones CW, Braz VA, et al. Risk factors for malnutrition among older adults in the emergency department: a multicenter study. J Am Geriatr Soc. 2017;65(8):1741–7.
Google Scholar
Pereira GF, Bulik CM, Weaver MA, Holland WC, Platts-Mills TF. Malnutrition among cognitively intact, noncritically ill older adults in the emergency department. Ann Emerg Med. 2015;65(1):85–91.
Google Scholar
Calf AH, Lubbers S, van den Berg AA, et al. Clinical impression for identification of vulnerable older patients in the emergency department. Eur J Emerg Med. 2020;27(2):137–41.
Google Scholar
Schuijt H, Oud F, Bruns E, et al. Does the Dutch Safety Management Program predict adverse outcomes for older patients in the emergency department? Neth J Med. 2020;78(5):244–50.
Google Scholar
Deschodt M, Devriendt E, Sabbe M, et al. Characteristics of older adults admitted to the emergency department (ED) and their risk factors for ED readmission based on comprehensive geriatric assessment: a prospective cohort study. BMC Geriatr. 2015;15(1):1–10.
Google Scholar
Nalbur İH, Sayhan MB, Oğuz S, Sayhan ES, Hüseyin S. Nutritional Situation Assessment of 65 Years Old Patient who Applicate to Emergency Department Acil Servise Başvuran 65 Yaş Üzeri Hastalarda Nütrisyonel Durumun Değerlendirilmesi.
Rarek MP, Meyer AM, Pickert L, et al. The prognostic signature of health-related quality of life in older patients admitted to the emergency department: a 6-month follow-up study. Aging Clin Exp Res. 2021;33(8):2203–11.
Google Scholar
Elias TC, Bowen J, Hassanzadeh R, Lasserson DS, Pendlebury ST. Factors associated with admission to bed-based care: observational prospective cohort study in a multidisciplinary same day emergency care unit (SDEC). BMC Geriatr. 2021;21(1):1–13.
Google Scholar
Gentile S, Lacroix O, Durand A, et al. Malnutrition: a highly predictive risk factor of short-term mortality in elderly presenting to the emergency department. J Nutr Health Aging. 2013;17(4):290–4.
Google Scholar
Lin C-F, Lin P-C, Hu S-Y, et al. Comprehensive Geriatric Assessment and Clinical outcomes in the older people at the Emergency Department. Int J Environ Res Public Health. 2021;18(11):6164.
Google Scholar
Saario EL, Mäkinen MT, Jämsen ER, Nikander P, Castrén MK. Screening of community-dwelling older patients by the emergency medical services: an observational retrospective registry study. Int Emerg Nurs. 2021;59:101078.
Google Scholar
Pulido I, Nunes C, Botelho A, et al. Comprehensive geriatric assessment of older patients and associated factors of admission to Emergency Departments in pre-covid 19 Era–A Portuguese study. Rev Esp Geriatr Gerontol. 2022;57(5):250–6.
Google Scholar
Tavenier J, Rasmussen LJH, Andersen AL, et al. Association of GDF15 with inflammation and physical function during aging and recovery after acute hospitalization: a longitudinal study of older patients and age-matched controls. Journals Gerontology: Ser A. 2021;76(6):964–74.
Google Scholar
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for Undernutrition in Geriatric Practice: developing the short-form Mini Nutritional Assessment (MNA-SF). J Geront. 2001;56A:M366–377.
Google Scholar
Vellas B, Villars H, Abellan G, et al. Overview of the MNA® – its History and challenges. J Nutr Health Aging. 2006;10:456–65.
Google Scholar
Elia M. The MUST Report. Nutritional screening of adults: a multidisciplinary responsibility. Development and Use of the Malnutrition Universal Screening Tool (‘MUST’) for adults. BAPEN; redditch, UK: 2003. Chairman of MAG and Editor advancing Clinical Nutrition, a Standing Committee of BAPEN.
Wilson M-MG, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, Diebold MR, Morley JE. Appetite Assessment: simple appetite questionnaire predicts weight loss in Community-Dwelling adults and nursing home residents. Am J Clin Nutr. 2005;82:1074–81. https://doi.org/10.1093/ajcn/82.5.1074.
Google Scholar
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36.
Google Scholar
Correia MITD. Nutrition screening vs nutrition assessment: what’s the difference? Nutr Clin Pract. 2018;33(1):62–72.
Google Scholar
Norman K, Haß U, Pirlich M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients Aug. 2021;12(8). https://doi.org/10.3390/nu13082764.
Laur C, Curtis L, Dubin J, et al. Nutrition Care after Discharge from Hospital: an exploratory analysis from the more-2-Eat study. Healthcare. 2018;6(1). https://doi.org/10.3390/healthcare6010009.
Beck AM, Kjær S, Hansen BS, Storm RL, Thal-Jantzen K, Bitz C. Follow-up home visits with registered dietitians have a positive effect on the functional and nutritional status of geriatric medical patients after discharge: a randomized controlled trial. Clin Rehabil. 2013;27(6):483–93.
Google Scholar
Ji T, Zhang L, Han R, et al. Management of Malnutrition based on Multidisciplinary Team decision-making in Chinese older adults (3 M study): a prospective, Multicenter, Randomized, controlled Study Protocol. Front Nutr. 2022;9:851590. https://doi.org/10.3389/fnut.2022.851590.
Google Scholar
O’Keeffe M, Kelly M, O’Herlihy E, et al. Potentially modifiable determinants of malnutrition in older adults: a systematic review. Clin Nutr. 2019;38(6):2477–98.
Google Scholar
Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional Risk Screening and Assessment. J Clin Med Jul. 2019;20(7). https://doi.org/10.3390/jcm8071065.
Guigoz Y, Vellas B. Nutritional assessment in older adults: MNA® 25 years of a screening tool & a reference standard for care and research; what next? J Nutr Health Aging. 2021;25:528–83.
Google Scholar
Dent E, Wright OR, Woo J, Hoogendijk E. O. Malnutrition in older adults. Lancet. 2023;401(10380):951–66.
Google Scholar
Lyu Y, Chen G, Shen L, Liu Y, Gao F, He X, Crilly J. Knowledge, attitudes, clinical practice and perceived barriers with nutrition support among physicians and nurses in the emergency department: a national cross-sectional survey. Int Emerg Nurs. 2021;55:100973.
Google Scholar
Lindorff-Larsen K, Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Group TS. N. Management and perception of hospital undernutrition—A positive change among Danish doctors and nurses. Clin Nutr. 2007;26(3):371–8.
Google Scholar
Mowe M, Bosaeus I, Rasmussen HH, Kondrup J, Unosson M, Rothenberg E, Irtun Ø. Insufficient nutritional knowledge among health care workers? Clin Nutr. 2008;27(2):196–202.
Google Scholar
Health Information and Quality Authority (HIQA). https://www.hiqa.ie/reports-and-publications/key-reports-and-investigations/report-review-nutrition-and-hydration-care
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–3270.
Google Scholar
Bech CB, Svendsen JA, Knudsen AW, Munk T, Beck AM. The association between malnutrition and dehydration in older adults admitted to a geriatric unit: an observational study. Clin Nutr ESPEN. 2023;57:598–605. https://doi.org/10.1016/j.clnesp.2023.08.011.
Google Scholar